|
I. CPD Needs Assessment
Moving Towards Mastery—A Needs Assessment of Online CPD Provision During the Pandemic
III. Building Capacity and Effective Teams
Beyond Grand! Grafting a Structured Reflective Tool to Hospital Rounds
Holding Braver Conversations: Interpersonal Conflict Simulations
How to Collaborate Successfully in Online Educational Programs for Latin America
Monitoring and Evaluating AI: Challenges and Practical Implications
Practice Assessment Tools for Medical Specialists—A Bridge to Quality Improvement
Developing a Patient Safety Culture Training Curriculum for Healthcare Professionals
Preparing Physicians to Lead Organizational Change
IV. Innovation and Adapting in Changing Times
A Call to Action: Committing to Diversity, Equity, and Inclusion in CPD
CPD Diversity Audit: Tracking and Reflecting on CPD Decisions for Advancing Justice
Regularly Scheduled Series (RSS’s)—Reimagined
Reimaging Bias: Making Strange with Disclosure
Success of Virtual Platform for an Established “Train the Trainer” Course
Perspectives and Innovation in Educational Design from the GAME Futurist Forums
Educational Needs for Infection Prevention and Control (IPC) for COVID 19 Pandemic in a Low Middle Income Country
Authors: Savithiri Ratnapalan, PhD, MBBS, Niranjala Perara, MD, MSc, Vitoria Haldane, PhD (C), MPH, Sudath Samraweera, MD, PhD, Xiaolin Wei, PhD
Institution: University of Toronto, Hospital for Sick Children
Background/purpose/inquiry question
Prior to developing educational materials on infection prevention and control (IPC) guidelines for Covid-19 pandemic management, we conducted this study to identify learning needs of health care workers (HCW) in Sri Lanka.
Theoretical framework(s)
Semi-structured interviews conducted using a grounded theory methodology
Methods
Sixteen participants including nine physicians (including three policy- makers responsible for COVID-19 pandemic management ), three nurses, two public health midwives and two support workers ( cleaning and transport staff) were interviewed.
Results/findings
Interview findings are described under three themes: HCWs workload; pandemic management guidelines and education provided; and guidelines and education desired. The pandemic increased staff workload for both in hospital and community HCWs; HCWs were provided with some form of IPC training but there were lapses in adherence; staff were interested in having easy to use desk guides, training videos and multimodal training.
Discussion
Our results highlight that a tailored approach to IPC education based on identified overall and key specific needs (such as training support staff) provides crucial information to improve HCW capacities in LMICs in response to either COVID-19 or future public health emergencies.
Limitation
The training needs identified in this study are from one LMIC country and in some regards are likely specific to the context in Sri Lanka. As such, the authors do not claim any generalizability.
Impact/relevance to the advancement of the field of CME/CPD
Our results show that many support staff have expanded scopes of practice and provide a significant amount services involving patient or patient environmental contact and need to be continuously educated along with other frontline staff on IPC practices.
Moving Towards Mastery—A Needs Assessment of Online CPD Provision During the Pandemic
Authors: Heather MacNeill, MD, MScCH (HPTE), Morag Paton MEd, Suzan Schneeweiss, MD, MEd, David Wiljer, PhD
Institution: University of Toronto, Toronto, Canada
Purpose/Problem Statement/Scope of Inquiry
COVID19 moved online CPD delivery from "nice to do" to something CPD providers "had to do", requiring additional skills and competencies. This study describes CPD providers’ comfort, resources, perceived advantages/disadvantages, and consensus on issues around privacy and copyright, in technology-enhanced CPD.
Approach(es)/Research Method(s)/Educational Design
A 26-item online survey was deployed through Qualtrics and piloted. The survey gathered information from CPD providers at the University of Toronto (UofT) and SACME about moving from face-to-face CPD delivery to virtual. Descriptive statistics were analyzed using SPSS. This work is informed by Bandura’s theory of self-efficacy, the technology acceptance model, and the community of inquiry framework. Evaluation/Outcomes/Discussion The survey had a 15.5% response rate. 81% felt confident to provide online CPD, but under half reported access to IT, financial, or faculty development supports. The most reported advantage to online CPD was reaching a new demographic, with virtual meeting fatigue the most reported disadvantage. There was interest in using collaboration tools, virtual patients, and augmented/virtual reality in future CPD delivery. There was inconsistent consensus on privacy and copyright issues.
Identified themes included 1) Social and learning norms in the online environment are evolving and contextual, 2) CPD providers recognize the importance of promoting active learning but need further training and resources to learn how to do this well online, 3) Accessible and safe learning environments are components of successful interactive online CPD programs and 4) Adequate preparation by learners, presenters, and providers is important for effective online CPD.
The necessity of COVID-19 helped develop a comfort level in providing online CPD, but further support is needed to develop best practices.
The response rate may limit generalization of the results, however the consistency in responses between UofT and SACME participants is reassuring.
Key Learnings for CME/CPD Practice
This research has implications for our collective ability to move towards best practices in CPD technology enhanced delivery. We need to pay attention to emerging issues such as evolving norms, interactivity, accessibility, and preparation while making sure we offer sufficient resources, including funding and faculty development to build best practices for the future.
Adoption of Telehealth by Clinical Teachers, Supervisors and Clinical Practitioners at McGill University and Teaching Hospitals: A Needs Assessment
Authors: Francesca Luconi, PhD, Beatrice Lauzon, Lalla L, Mercer G, Levin L, Arsenault M, Elizov M, Jarvis C.
Institution: McGill University
Problem statement
Telehealth predates the Covid-19 pandemic1,2 and evidence suggests that it can expand critical care, speed emergency care decisions, replace face-to-face care and reduce exposure to infections3.
The WHO defines telehealth as: “[t]he delivery of healthcare services (…) by all healthcare professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research, and evaluation, and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities”4
Although the use of telehealth has increased worldwide in response to the Covid-19 pandemic, little is known about the needs of academic leaders and clinical practitioners in adopting telehealth in Quebec, Canada.
Our aim was to investigate perceived and unperceived needs of practicing physicians in Quebec and to identify barriers and enablers to using telehealth (TH).
Research Method
A needs assessment (NA) is a systematic process of collecting and analyzing data on the target audience’s educational needs5 and a comprehensive needs assessment is crucial to planning and developing relevant continuing professional development6. We collected data via two online surveys exploring physicians’ perceived needs, which can be defined as what learners think they want to learn6. One survey (S1) targeted academic leaders (i.e., clinical chairs and division directors in departments of medicine) while the other surveyed practicing physicians (in their roles of teacher at undergraduate or post-graduate levels, supervisor of trainees and/or clinical practitioner) affiliated with McGill University and its teaching hospitals (S2).
Unperceived needs can be defined as “I do not know what I do not know”6. These were investigated via a report on medico-legal cases and advice calls involving telehealth (from the Canadian Medical Protective Association or CMPA) as well as questions about participants’ reported challenging cases in diagnosing and treating patients using TH (from S2).
Descriptive statistics, deductive thematic analysis and triangulation of sources were conducted on these data.
Outcomes and Discussion
S1 (conducted in 2020) included a convenience sample of 20 clinical chairs (60%) and division directors in departments of medicine (40%) representing 12 medical specialties. Most respondents anticipated a high uptake of TH for teaching and supervision of trainees.
S2 (conducted in 2021) included 250 physicians of which 53% were family physicians and 45% other specialists. Their demographic profile covered a range from more experienced to less experienced professionals (55.3% ≥16 years 20.4% ≤5 years of experience as clinicians).
Beginning in March 2020, adoption of TH was high across teachers, supervisors and clinicians. The most frequently reported role was clinical practitioner (64.8%) where use of telehealth ‘often’ or ‘very often’ increased from 10.1% to 88.3%.
Increased use of telehealth was also reported by the CMPA which received 970 advice calls related to telemedicine between January 1st, 2019 and May 2020, with 70% of the calls were made in the period of March – May 2020. 69% (of a subsample n=478 calls where TH was the main reason for the call) focused on the adoption of TH to continue duty of care for existing patients during the pandemic and 64% reported using the telephone for consultations.
Before the pandemic (2015-2019) the CMPA reported on 45 medico-legal cases involving the use of TH, reporting on influencing factors at the individual, team and systemic levels. Delayed diagnosis when using TH was the most reported challenging case by our participants in S2. Their needs during the pandemic coincided with unperceived needs reported by the CMPA prior to March 2020. One of the most frequently reported factors at the provider level in both sources was provider deficiencies with regards to selecting appropriate technology for patient care. (Inadequate monitoring and follow-up were also reported in S2, while procedural violations were reported as a factor in the CMPA analyses.) At the team level major factors were communication breakdown (with patients and/or other physicians, identified by S2 and CMPA), as well as deficient record keeping (CMPA only). While few system level factors were reported, both sources reported that lack of/inadequate office policies, procedures or practices as a factor at this level.
Triangulation of sources indicated some consistency with regards to major barriers to and enablers of the adoption of TH. At the individual/provider level, perception of impersonal care/interaction and privacy/security concerns were barriers reported across more than one source. Organizational barriers reported across 2 or more sources included outdated hardware, restricted remote access to medical records and electronic charting, as well as infrastructure. Top enablers across ≥2 sources included TH’s safety as well as its ‘timeliness’. Thematic analyses suggest that in clinical practice TH was usually adopted when physical exam was not required, for follow-ups and for care of specific types of patients; limited patient access to TH was due to lack of or limited digital health literacy. These results suggest the need for implementation of strategies to address and mitigate challenges for vulnerable patients.7,8
In conclusion, physicians’ use of TH for patient care has greatly increased in response to Covid-19 yet important barriers remain. Identified gaps and facilitating factors might trigger sustainable change at multiple levels if identified needs can be met. Limitations of our study include the timing of data collection, which varied across sources. Differing timing could therefore have affected triangulation of results. In addition, medico-legal cases are not representative of all physicians’ use of TH and generalizability of findings may be limited due to the use of a convenience sample.
Learning AI, Making it Real: A Qualitative Study of the Needs of Medical Educators for Artificial Intelligence Program Development
Authors: David Wiljer, PhD, Mohammad Salhia, Med,Sarmini Balakumar, BSc, Tharshini Jeyakumar, MHI, Sarah Younus, MPH, Rebecca Charow, MSC, Melody Zhang, MA, Elham Dolatabadi, PhD, Azra Dhalla, MBA, Caitlin Gillan, PhD, Dalia Al-Mouaswas, BSC, Jacqueline Waldorf, EMBA, Jane Mattson, MLT, Megan Clare, MA, Walter Tavares, PhD, Ethan Jackson, PhD
Institution: University of Toronto, Toronto, ON, Canada
Purpose/Problem Statement/Scope of Inquiry
The National Academy of Medicine highlight the need for developing, deploying, and evaluating AI educational programs to support the safe, effective and sustainable use of AI in clinical practices. This study informs the third phase of a multi-stepped approach to accelerating the appropriate adoption of AI in health care, and is informed by the Knowledge-to-Action framework. Specifically, it aimed to understand the current landscape of AI education for health care professionals and recommendations for future education program development.
Approach(es)/Research Method/Educational Design
A qualitative approach was taken to explore the needs of educators and learners of AI education programs targeted at clinicians, leaders and scientists in healthcare. Virtual semi-structured interviews informed by the Kirkpatrick Barr (for learners) and RE-AIM (for educators) frameworks were conducted. These interviews were recorded, transcribed, and analyzed using inductive thematic analysis.
Evaluation/Outcomes/Discussion
A total of 17 participants were recruited for the study: 10 educators and 7 learners. Three major themes emerged about AI education approaches, which were valued by both learners and educators: (1) practical experiences to support the transfer of learning, (2) multidisciplinary approaches to curriculum development and course delivery, and (3) balancing learner needs and promoting engagement through a learner-centered pedagogy when developing AI education programs. The first theme highlighted the importance of hands-on activities such as workplace learning, debates, and group-based learning and access to appropriate resources (i.e., health data). The second theme focused on co-designing the curricula collaboratively with experts from various disciplines as well as providing opportunities to engage in multidisciplinary learning to replicate real-world scenarios and fit with industry demands. The last theme stressed the importance of selecting an appropriate mode of delivery and continuously evaluating the program and learners.
This study was presented at SACME as an oral presentation, under the category of CPD needs assessment. The presentation was given to approximately 200 attendees. The study received positive feedback from the audience, with several individuals raising thoughtful questions and comments that energized the conversation. For instance, one question revolved around the topic of patient involvement in AI adoption and implementation. There was curiosity on whether research on AI has gone beyond clinicians and researchers to include patient perspectives, such as patient acceptability towards AI, eHealth or digital eHealth initiatives. Although patients and patient advocates have been included in various aspects of our study project, including: (1) a steering committee where patients were engaged during the planning and development of our project, (2) a needs assessment interview with patients to understand their perspectives and attitude towards AI, as well as (3) patient participation in our AI certificate program, many issues must still be addressed. For instance, a gap in the literature still exists on patient consent with AI; further research should examine this in relation to care delivery.
Key Learnings for CME/CPD Practice
The findings from this study can be used to advance CME/CPE through the development of practical AI education programs in healthcare. In partnership with The Michener Institute of Education and the Vector Institute, we have developed an evidence-based education program, “AI for Clinical Champions” that will empower a Canadian workforce with the appropriate skills, knowledge, and capabilities to adapt and implement AI into clinical practice and healthcare organizations. Future directions include the continuous evaluation and improvement of education programs to ensure the effectiveness and relevance for learners. Furthermore, to encourage discourse within the research, clinical, and general community, engagement activities such as national or international symposiums will be held to engage a greater audience in conversations about AI in health care.
Impact of Culture on Combatting Burnout and Stress in the Field of Laboratory Medicine
Authors: Lotte Mulder, PhD, Edna Garcia, MPH, Joseph S. Sirintrapun, MD, Iman Kundu, MPH
Institution: American Society for Clinical Pathology
Purpose/Problem Statement/Scope of Inquiry
Little research has been conducted concerning organizational culture issues impacting the field of pathology and lab medicine, especially when it comes to well-being and burnout. When the COVID-19 pandemic happened, the laboratory field was profoundly impacted. This prompted us to identify the connection between burnout, the pandemic, DEI, and organizational culture to further support our workforce.
The overall purpose of this study is to understand the unique pressures of COVID-19 in pathology and laboratory medicine, develop strategies to mitigate burnout and toxic organizational cultures, and advocate for and create resources to improve DEI and wellness within the laboratory.
Approach(es)/Research Method(s)/Educational Design
To capture data about culture, burnout, DEI, and wellness from medical laboratory professionals during the pandemic, the study utilized a cross-sectional survey design. Because the pandemic continues to affect the field in so many areas, this study has become a longitudinal study. The theoretical framework used in this study is based on the interrelationship between burnout, DEI, and organization culture and its components, such as structures, systems, and behaviors.
This study was divided into two phases. Phase 1 was launched in August 2021, with an online survey that was deployed for one week. There were 2609 respondents, of which 86% were laboratory professionals, 5% pathologists, and 2% trainees. We used a cross-sectional survey design for both surveys.
In terms of ethnicity, 75% identified as White/Caucasian, 5% as Black or African American, 9% as Asian or Pacific Islander, 6 % as Latinx, 0.6 % as Native American, 1% as West Asian, and 3.4% as other.
Limitations of this phase include a short survey deployment period, a low number of pathologist and trainee participants, and a lack of a diverse group of participants. There is also the potential for participant self-selection bias.
To mitigate these limitations, Phase 2 had a longer deployment period of one month and participants from a more diverse audience were targeted, including pathologists, trainees, and participants who do not identify as White or Caucasian. This phase also enlisted help from eight partner specialty organizations in the field of laboratory medicine to increase the reach of the survey. Finally, 31 additional questions were added to the initial survey to get more detailed information on the impact of DEI, the pandemic, burnout, and wellness. Repeat participants were prompted to only answer the additional questions. This time, there were 3,544 participants, of which 10.41% were repeat participants from our August survey. Of the 3,175 new participants, 82% were laboratory professionals, 7% were pathologists, and 2% were trainees.
In terms of ethnicity, 77% identified as White/Caucasian, 5% as Black or African American, 1% as African, 8% as Asian or Pacific Islander, 5% as Latinx, 1% as Native American, 1% as Middle Eastern/West Asian, and 3% as other.
Evaluation/Outcomes/Discussion
Phase 1 Findings:
The initial phase of the study found that current burnout rates in the field of pathology and laboratory medicine were especially high. 52.5% of laboratory professionals, 46% of pathologists, and 27.10% of trainees indicated that they are experiencing burnout in the present and in the past. Additionally, 23.8% of laboratory professionals, 13.5% of pathologists, and 6.3% of trainees indicated that they are experiencing burnout in the present but not in the past.
We asked those who indicated that they were currently experiencing burnout if the COVID-19 pandemic caused or worsened their burnout. The pandemic caused burnout in 27% of laboratory professionals and 10% of pathologists and worsened the burnout of 51% of laboratory professionals and 30% of pathologists.
Of the factors contributing to participants’ burnout, laboratory professionals most frequently indicated the following factors: increased workload (60.4%), COVID-19 pandemic (54.6%), poor management culture (50.1%), work-related stressors (44.1%), and toxic work environment (31.4%). Pathologists indicated works related stressors (40.9%), increased workload (40.2%), poor management culture (37.8%), poor work-life balance (37%), and a toxic work environment.
Despite the high number of participants who identified as White/Caucasian (75%), 16.5% of pathologists and 7% of laboratory professionals stated that discrimination, sexism, racism, and microaggressions were contributing factors to their burnout. Additionally, 5.5% of pathologists and 7.8% of laboratory professionals mentioned grief and/or trauma as causes.
Phase 2 Findings:
The second phase of the study found that current burnout rates remained similar to the results of the first phase, with one significant difference. Present and past burnout rates among trainees increased from 27.10% to 44%. Additionally, 50% of laboratory professionals and 44% of pathologists indicated that they are experiencing burnout in the present and in the past. Additionally, 26% of laboratory professionals, 15% of pathologists, and 5% of trainees indicated that they are experiencing burnout in the present but not in the past.
The main contributing factors of burnout in phase two were the COVID-19 pandemic (66%), increased workload (64%), poor management culture (50%), work-related stressors (50%), and poor compensation (46%). In terms of DEI factors, 9% of all participants indicated that grief/trauma contributed to their burnout and 6.8% of participants mentioned discrimination, racism, sexism, and microaggressions.
Key Learnings for CME/CPD Practice
Pathology and laboratory medicine play a crucial role in the nation’s health care system and the well-being of patients. The more data are available about how burnout impacts laboratory medicine, the more targeted and laboratory-specific solutions can be created. Burnout is a preventable, organizational phenomenon; this study offers solutions and recommendations to mitigate burnout in the field of laboratory medicine
The study identified differences in burnout rates between types of medical laboratory professionals, as well as between different demographics such as ethnicity. Results showed that organizational culture is a cause and a potential remedy to overcome burnout in the laboratory. The more open, inclusive, and well-staffed organizations are, the less likely medical professionals are to experience burnout.
Burnout: An Example of an Inter-relationship Between Health and Learning
Authors: Juliamaria Coromac-Medrano, BS, Nathaniel Williams, BA, Michael V. Williams, PhD, and Betsy White Williams, PhD, MPH
Institution: Professional Renewal Center®/Wales Behavioral Assessment
Purpose/Problem Statement/Scope of Injury
Medical professionals are met with immense pressure and responsibility being at the front line of patient care. They also face ongoing stressors due to the continuous exploration for medical knowledge within the field of medicine, increasing administrative burdens, increasing patient demand, and a disproportionate low number of available physicians to treat patients (Williams et al., 2018).
With these external stressors in mind, a study conducted by Stewart and Arora (2019) found that nearly 50% of physicians report symptoms of clinical burnout, with the highest rates of burnout reported amongst family medicine, general internal medicine, and the emergency medicine specialties. Burnout has been associated with medical errors (Stewart and Arora, 2019), failure to maintain the expectations of professionalism in medicine and can be associated with poorer performance on neuropsychological tests (Williams et al., 2018).
We hypothesized that physicians who report high rates of burnout would perform more poorly on memory subtests of the California Verbal Learning Test 2nd Edition (CVLT-II) compared to physicians without high rates of burnout. Furthermore, we explored which of the three dimensions of the MBI (emotional exhaustion, depersonalization, and reduced personal accomplishment) correlated most strongly with impairments in memory scores.
Approach(es)/Research Method(s)/Educational Design
This study was reviewed and determined exempt by the WCG IRB. Data from a total of 280 clients were obtained from the Professional Renewal Center’s (PRC®) data sets containing information about clients from the time interval 2015-2019. All clients in the data set are physicians.
Subjects: This sample included 249 males and 31 females. The average age of the sample was 51.11 years.
Measure: Memory performances were measured with the California Verbal Learning Test, a test that requires the participant to learn and recall lists of words presented over several trials. Four of the memory subtests, short and long delayed cued and free recall, were analyzed. The free recall condition requires the participant to list the words they remember while in the cued recall condition the psychometrist provides a categorically-related prompt (cued recall).
We evaluated burnout using the Maslach Burnout Inventory Human Services Survey (MBI-HSS). The MBI-HSS captures three dimensions of burnout: emotional exhaustion, depersonalization, and personal accomplishment self-report. Emotional exhaustion is described as feeling emotionally overextended and exhausted by one’s work, depersonalization is the unfeeling and impersonal responses towards patients under the physician’s care, and reduced personal accomplishment is described as feelings of competence and successful achievement in one’s work with people (Maslach et al., 1997).
There are nine questions in the emotional exhaustion dimension, five in the depersonalization dimension, and eight in the reduced personal accomplishment dimension (Maslach et al., 1997). It is based on a six-point rating scale: Depersonalization (Low (0-6), Moderate (7-12), High (>27)), Emotional Exhaustion (Low (0-16), Moderate (17-26), High (>27)), Personal Accomplishment (Low (39)) (Dyrbye et al., 2009 & Lim et al., 2019).
Data Analysis: With this data set, a step-down regression model was utilized. Each dimension of burnout (emotional exhaustion, depersonalization, and personal accomplishment) was regressed on each recall section of the CVLT-II. The following parameters were regressed onto each CVLT subtest’s: MBI Emotional Exhaustion, MBI Personal Accomplishment, MBI Depersonalization, and the interactions between all three dimensions. The scores for each dimension were determined by the questions that fell under each category in the triad model
The results of the regression indicated that emotional exhaustion and to a lesser extent, depersonalization were the most active predictors of memory performance. The regression of emotional exhaustion onto the four memory subtests displayed significant results. Depersonalization was only significant for short delay free recall. Cued recall memory was the most sensitive of memory types. Free recall was found to be associated with the poorest performance with higher levels of emotional exhaustion. This means that clients who reported higher levels of emotional exhaustion had significant difficulty remembering the list of words without a prompt cue.
Evaluation/Outcomes/Discussion
Burnout has been linked to changes that undermine physicians’ connections with patients and their colleagues, a decreased sense of motivation, interference with work-life integration (Amsten and Shanefelt, 2021). The uncontrollable stress in a physician’s environment that leads them to reporting burnout may impair the functioning of the prefrontal cortex (Amsten and Shanefelt, 2021 secondary to uncontrolled stress which can contribute to high levels of norepinephrine and dopamine impairing prefrontal cortex cognitive functions such as working memory.
From a cognitive perspective, cognitive load theory may provide insight into how burnout affects physician’s memory. This theory states task completion relies on an interplay between sensory inputs, “long-term memory acting as a repository of acquired knowledge and skills, with working memory as the intermediate stage, attributing meaning to sensory information,” and transferring the new information into long term memory (Iskander, 2018). Cognitive load directly refers to the amount of working memory that is devoted to synthesizing novel information and expanding current mental models to absorb new information (Harry et al., 2021).
Physicians are responsible for engaging in lifelong learning and maintaining their currency to achieve the best patient care. It is important to consider the potential implications of physician burnout on their ability to acquire new information and in turn the implication of that for CME/CPD.
Key Learning for CME/CPD Practice
Burnout is associated with aspects of learning and memory.
Learning requires working and active memory recall and retrieval. Clearly remembering new information is important to a physician’s remediation. There is evidence that assessing burnout-linked memory issues has implications for the pedagogical approach to remediating physicians.
Less effortful strategies such as cued recall and recognition may be a better measure of retention in physicians suffering from burnout.
References:
Amsten, F.T. & Shanafelt, T. (2021). Physician Distress and Burnout: The Neurobiological Perspective. Mayo Clinic Proceedings, 96(3), 763+ https://link.gale.com/apps/doc/A657476740/AONE?u=ksstate_ukans&sid=summon&xid= 9b70f63e
Dyrbye, West, C.P., & Shanafelt, T. D. (2009). Defining Burnout as a Dichotomous Variable. Journal of General Internal Medicine: JGIM, 24(3), 440-440. https://doi.org/10.1007/s11606-008-0876-6
Harry, E., Sinsky, C., Dyrbye, L. N., Makowski, M. S., Trockel, M., Carlasare, L. E., West, C. P., & Shanafelt, T. D. (2021). Physician Task Load and the Risk of Burnout Among US Physicians in a National Survey. Joint Commission Journal on Quality and Patient Safety, 47(2), 76-85. https://doi.org/10.1016/j.jcjq.2020.09.011
Iskander, M. (2019). Burnout, Cognitive Overload, and Metacognition in Medicine. Med.Sci.Educ. 29, 325-328. https://doi.org/10.1007/s40670-018-006545
Lim, Ong, J., Ong, S., Hao, Y., Abdullah, H. R., Koh, D. L., & Mok, U. S. M. (2019). The Abbreviated Maslach Burnout Inventory Can Overestimate Burnout: A Study of Anesthesiology Residents. Journal of Clinical Medicine, 9(1), 61. https://doi.org/10.3390/jcm9010061
Maslach, C., Leiter, M., & Jackson, S. E. (1997). The Maslach Burnout Inventory. The Scarecrow Press.
Stewart, N. H. & Arora, V. M. (2019) The Impact of Sleep and Circadian Disorders on Physician Burnout. Chest, 156(5), 1022-1030. https://doi.org/10.1016/j.chest.2019.07.008
Williams, B., Flanders, P., Welindt, D., & Williams M. V. (2018). Importance of neuropsychological screening in physicans referred for performance conerns. PLoS ONE, 13(11). https://doi.org/10.1371/journal.pone.0207874
Developing a Mentorship Culture: Perspectives of Departmental Leadership on a Faculty Mentorship Program - A Qualitative Study
Authors: Michael Ren, BSc, Chloe Chan, Simrit Rana, Dorothy Choi, BSc, Umberin Najeeb, MD, Mireille Norris, MD, Simron Singh, MD, Karen EA Burns, MD, Sharon Straus, MD, Gillian Hawker, MD, Catherine Yu, MD
Institution: University of Toronto
Purpose/Problem Statement/Scope of Inquiry
Physician burnout is rising, and the issue is particularly complex among physicians in academic medicine. These physicians have multiple and often competing responsibilities because in addition to providing patient care, they are also involved in research and medical education (1). A potential strategy to mitigate this burnout is through faculty mentorship. There are many benefits associated with faculty mentorship including increased self-efficiency, greater career satisfaction, and higher faculty retention (2). The Department of Medicine at the University of Toronto Temerty Faculty of medicine has created faculty mentorship program, however a process evaluation and an assessment on faculty mentorship needs is still lacking. Thus, we sought to understand the strengths and limitations of the department’s faculty mentorship program and identify opportunities for enhancement from the perspective of departmental leadership.
Approach(es)/Research Method(s)/Educational Design
Departmental Divisional Directors (of divisions with more than 10 faculty members), Vice Chairs, and two divisional mentorship facilitators were interviewed using a semi-structured guide exploring barriers and facilitators to mentorship, and current mentoring processes. Interviews were audio-recorded, transcribed, and analyzed using qualitative descriptive approach.
Evaluation/Outcomes/Discussion
Three emerging themes were identified: 1) Establishing a culture that encourages and values mentorship is paramount, and it necessitates a multilevel approach, 2) Mentorship barriers exist at various levels within an academic institution and 3) A tension exists between standardization vs individualization of mentorship processes.
There are various implications from these findings. In order to begin cultivating a mentorship culture, support and engagement is needed from all individuals within an academic institution. It involves faculty members understanding the value of mentorship as well as the academic institution recognizing its value and taking tangible steps to acknowledge and reward effective mentorship. Furthermore, when the department creates and implements mentorship processes, they need to be clear and flexible to address divisional and individual faculty nuances.
Key Learnings for CME/CPD Practice
This study highlights the challenges of addressing the diverse mentorship needs of physicians in academic medicine. It also outlines strategies to promote a culture of mentorship, with an emphasis on ensuring that individuals within an academic institution value and are engaged in mentorship activities, and that actionable steps are taken to recognize as well as maintain these values.
Relationship among Professionalism Concerns, Capacity, and Duration of Remediation
Authors: Hailey Amro, BA; Nathaniel Williams, BA; Michael Williams, PhD; Betsy W. Williams, PhD, MPH, FSACME
Institution: Professional Renewal Center® and Wales Behavioral Assessment
Purpose/Problem Statement/Scope of Inquiry
Physician performance failures are not rare but pose substantial threats to patient welfare and safety and can be usefully thought of as symptoms of underlying disorders and/or other contributory factors (Leape & Fromson, 2006). Past research has suggested that remediation can be an effective way to address physicians with problematic behaviors (Moskowitz, 2010).
The Environmentally Valid Learning Approach offers a framework within which to approach the remediation of physicians. The framework suggests that remediation of problematic behavior is dependent on multiple individual factors and considers other contributory factors, areas of knowledge/skills deficits, best approaches to addressing deficiencies, and elements that need to be in place to foster implementation and maintenance of gains. Capacity is one of the elements of the framework. Capacity is characterized by biopsychosocial factors and includes undiagnosed medical conditions, psychiatric conditions, and various social issues. In this study we focus specifically on capacity measures and how they relate to remediation length.
Approaches/Research Methods/Educational Design
Subjects: Data collected were from 103 physicians referred for remediation to a center in the Midwest. Part of the remediation process involves the collection of data that are used to inform the remediation approach. The physicians were independently identified as performing below expectations in the ABMS core competency area of professionalism prior to their arrival at the center. Specific behaviors of concern included difficulty establishing and maintaining appropriate boundaries with patients or staff, difficulty establishing appropriate boundaries around prescribing, behaviors that was disruptive to the functioning of the system, compliance issues, and health and well-being concerns (for example burnout).
Data Collection
Several self-report surveys were used to provide data that provided information about biopsychosocial functioning. Specific measures included the Ten-Item Personality inventory (TIPI) was used to collect data on personality factors, the DSM-V Anxiety Scale was used to determine the presence of anxiety, the Maslach Burnout Inventory (MBI) was used to assess for burnout, the DSM-V Anger Scale was used to screen for anger while the DSM-V Sleep Scale was used to determine the quality of sleep received by our participants. Reported age was used to determine career point. The change questionnaire version 1.2 provided data on the participant’s understanding of the need to change. Length of remediation was operationalized as the participant’s dates of attendance in the program.
Analysis
This study was deemed to be exempt by WCG IRB.
Results
Physicians ranged in age from 23-69. Median age of the group was 49.06 years. Diagnostic = 56 and Procedural = 47.
A multivariate linear regression was used to analyze our data. The seven variables (personality, anxiety, burnout, anger, sleep, age, and belief in a need to change) together were correlated to the length of remediation. It was found that those seven variables together accounted for nearly half of the variance (R2 value of 0.48). Those results were found to be significant.
Evaluation/Outcomes/Discussion
Results are consistent with the EVLA framework and highlight the importance of utilizing a multifactorial approach to behavioral change. Consistent with the broader literature and our earlier work, current results support the importance of biopsychosocial factors; for physicians to effectively learn and benefit from the content of the education within remediation, individual physician factors such as mood, burnout and physiological aspects need to be considered and addressed. Thus, while the acquisition of new knowledge and skills is an important part of a remediation process, knowledge and skills acquisition alone are not necessarily sufficient to fully remediate a physician with performance issues. This view is consistent of that of Durning (2011) and colleagues in their work with trainees. They discussed the importance of identifying and understanding the proximal causes of trainee underachievement, as without doing so it is difficult to pinpoint the most effective ways to assist trainees in improving their performance.
Key Learning for CME/CPD Practice
In relation to continuing medical education, our study suggests that success in a remedial learning application would be most effective if it contains a learner centric and multifactorial pedagogical approach to remediation as multiple factors are relevant to success and efficiency of the remediation process. Recognizing the potential contribution of biopsychosocial factors is important as remediation is less effective if such factors are not being addressed.
References
Durning, S., Cleary, T., Sandars, J., Hemmer, P., Kokotailo, P., & Artino, A. (2011). Perspective: Viewing "strugglers" through a different lens: How a self-regulated learning perspective can help medical educators with assessment and remediation. Academic Medicine, 86(4), 488-495.
Leape, L. L. & Fromson, J. A. (2006). Problem doctors: is there a system level solution? Annals Internal Medicine, 144(2), 107-115.
Moskowitz, P. S. (2010). RE: “Beyond substance abuse: Stress, burnout, and depression as causes of physician impairment and disruptive behavior”. Journal of the American College of Radiology, 7(4), 313-314.
Williams, B. W. & Williams, M. V. (2020). Understanding and remediating lapses in professionalism: Lessons from the island of last resort. The Annals of Thoracic Surgery, 109(2), 217-324.
Back To TopBuilding Capacity and Effective Teams
Adapting the Deteriorating Patient Simulation Method: Notes on the Feasibility and Acceptability of a Virtual Mental Health Simulation
Authors: Sanjeev Sockalingam, MD, MHPE, Noah Brierley, BA, Amanda Gambin, PhD, Thiyake Rajaratnam, MSc, Anne Kirvan, MSW, Michael Mak, MD, Chantalle Clarkin, PhD, Stephanie Sliekers, MEd, Fabienne Hargreaves, MA, Sophie Soklaridis, PhD, Allison Crawford, MD, PhD
Institutions: The Centre for Addiction and Mental Health, University of Toronto
Purpose
Continuing professional development (CPD) programs in mental health are critical to building primary care teams’ capacity in mental health care. However, healthcare professionals often report barriers such as access to CPD and cost which limit uptake. Deteriorating Patient Simulation (DPS) is a team-based simulation activity that aims to mimic real-life medical situations that deteriorate over time. It involves an instructor acting out a patient scenario that deteriorates as the simulation progresses, and requires the learners to determine the appropriate steps to stabilize the patient. Throughout the process, the instructor facilitates the deterioration while simultaneously offering content knowledge. DPS was originally developed to support medical trainees in emergency medicine; the overall goal of this simulation activity is to promote learning by eliciting evidence based decision-making in a realistic scenario. DPS has not been used in a virtual setting or within a mental health context; as such, this study aimed to evaluate the feasibility and acceptability of a virtual mental health DPS educational activity with primary care teams.
Approach
The study was conducted in two phases: Phase 1 focused on the development of patient scenarios and a competency checklist as well as the feasibility and acceptability of delivering the simulation virtually. Phase 2 sought to refine the checklist and evaluate inter-rater reliability. During both phases, post-DPS focus groups were conducted to understand participants’ perceptions of the activity.
Two patient scenarios were developed using an interprofessional collaborative approach; evidence-based best practice guidelines were used to develop scenarios focused on a major depressive episode and suicide risk assessment. Each scenario had a unique algorithm for deterioration based on the teams’ decision-making. The competency checklist was developed by content expert review including the primary investigators and mapped to case scenario goals and objectives.
Participants were previous participants of ECHO Ontario Mental Health at CAMH and University of Toronto. Generally, participant groups consisted of at least 1 prescribing professional (i.e. MD, NP) and 2 other healthcare professionals. DPS sessions were delivered via Zoom and were typically 2 hours in duration: the 60-minute DPS activity was followed by a facilitator-led debrief (30 minute) and a focus group (30-minute). Participant performance was scored by a third party rater using the competency checklist developed by the team.
Evaluation
Seventeen (17) healthcare providers (3 MD, 3 NP, 5 SW, 2 RN, 2 other) participated across 6 DPS sessions. Moderate inter-rater reliability was established for the DPS checklist (66% agreement). Focus group data highlighted barriers and facilitators to the activity. Participants responded positively to the structure and facilitation of the activity, and emphasized the simulation-based feedback from the post-activity debrief as integral to their learning. The DPS activity was described as valuable and appropriate for skill building, and the team-based nature of the activity provided an important interprofessional lens to patient management. Participants noted time constraints, as well as the formation of “artificial teams” specifically for this activity as challenges.
Key learnings for CME/CPD Practice
This pilot study provides evidence to support the potential use of virtual DPS as an accessible, low barrier, CPD activity to increase provider competency in mental health clinical decision-making. Further development of this activity could include use as an educational assessment tool, and to increase mental healthcare capacity in primary care teams.
Beyond Grand! Grafting a Structured Reflective Tool to Hospital Rounds
Authors: Sam J. Daniel, MD, MSc, FRCSC, Jane Tipping, MADEd, MCC
Institution: McGill University, Federation of Medical Specialists of Quebec, University of Toronto
Purpose/Problem Statement/Scope of Inquiry
In many institutions, grand rounds are a weekly educational activity and a time-honored tradition. Unfortunately, hospital-based grand rounds lack uniformity in value for the learners. Our goal was to make these group learning activities more conducive to a change in the clinicians’ performance by increasing critical thinking and enhancing engagement in rounds using a simple, structured, reflection tool.
Approach(es)/Research Method(s)/Educational Design
A reflection tool was systematically grafted after each grand rounds. The tool was based on Borton’s model of reflection (description, analysis, synthesis). It guided participants to reflect on their learning, by identifying a concrete enhancement in their practice, reflecting on barriers and facilitators, and stating a strategy and a timeline for implementation. A focus group was surveyed as to their experience with this tool through a structured interview.
Evaluation/Outcomes/Discussion
To date over 300 reflection tools have been collected. 80% of the participants felt that the grand rounds were relevant to their practice.
The most common barriers to implementing changes were time, followed by human resources and equipment issues.
Interviewees listed 4 key aspects of learning upon which the reflective survey touched:
- Encouraging critical thinking,
- Encouraging reflection,
- Engaging learners, and moving beyond passive learning, and
- Increasing the likelihood of application to practice.
Adding a reflection tool to grand rounds was successfully implemented. Participants valued the survey in reinforcing key concepts and integrating these concepts into practice. This tool continues to be popular 2 years after its deployment and is extending to other centres.
Facilitators included making the tool available immediately after rounds, and having champions participate and advocate for the tool.
Key Learnings for CME/CPD Practice
Adding a reflection tool, after grand rounds can transform CPD for group learning activities into active learning and allows participants to immediately initiate a Deming cycle with the identification of a change, and an action plan to implement it.
Holding Braver Conversations: Interpersonal Conflict Simulations
Authors: Trung Do, RN, BN, Kamini Kalia, RN, MScN, CPMHN(C), Stephanie Sliekers, Med, Tucker Gordon
Institution: University of Toronto, Centre for Addiction and Mental Health
Purpose/problem statement
During the COVID-19 pandemic, retention of clinicians has been priority, which has placed additional pressure on healthcare teams to work effectively and cohesively together. Education for new hires about how to handle challenging conversations with their peers can reduce experiences of interpersonal conflict, improve team collaboration, and resiliency.
Methods/Approach(es)
Utilizing the ERASE Framework, Cognitive Rehearsal Training, and Simulation teaching methods, an educational module for interprofessional teams was developed for newly hired clinicians. The training was designed to facilitate application of interpersonal conflict resolution skills with their colleagues utilizing role plays. A quality improvement framework was utilized using rapid review cycles to make quick and iterative improvements to education based on feedback.
Outcomes/Findings
Participants provided structured feedback in the form of in-person and post-session evaluations. Participants reported feeling supported by the organization as it was perceived by learners as an organizational priority. Participants also reported that the content was relevant and that they received guidance on how to respond to difficult situations as the scenarios were seen to be likely to arise in the workplace.
Discussion
A multi-pronged strategy is required to address issues of interpersonal conflict in interprofessional teams. These sessions highlight the need to also create structures and supports for faculty who deliver the education.
Barriers/facilitations
There are opportunities to strengthen the delivery method utilizing different types of simulation technology.
Key Learnings for CME/CPD Practice
Interpersonal conflict impacts all clinical roles and healthcare leaders have an opportunity through the use of simulation to offer options that that cultivate psychologically safe environments and confidence to have braver conversations.
How to Collaborate Successfully in Online Educational Programs for Latin America
Authors: Alvaro Margolis, MD, MS, Jann Balmer, PhD, RN, Steven Kawczak, PhD
Institution: EviMed (AM), University of Virginia (JB), Cleveland Clinic (SK)
Purpose/Problem
International collaborative programs in CME/CPD are of interest for many North American institutions. However, they pose different types of challenges, in terms of educational design, accreditation, convening or evaluation, but also in the need to address cultural and language barriers in order to be successful.
Latin America is a large and heterogeneous middle-income region, with one million physicians. One third of the region, by several counts, is Brazil, where Portuguese is spoken, while the rest of the countries speak Spanish. This dynamic creates an opportunity for online activities to be tailored to learner characteristics regionally and delivered in the two main native languages of the region.
The University of Virginia Office of Continuing Medical Education has been involved in web-based and innovative continuing education for physicians, nurses and healthcare professionals for over thirty years. The Center for Continuing Education at Cleveland Clinic is dedicated to providing a wide array of quality continuing medical education opportunities to medical professionals throughout the world. EviMed is a company that provides multilingual online programs for healthcare professionals across the Americas.
The COVID-19 Pandemic accelerated the collaboration between each of the two North American organizations and EviMed, and with other Latin American academic partners. The authors describe their experience in international collaborative educational programs for Latin America, in order to help other parties reflect on their own challenges and path towards the implementation of international programs with developing countries and regions.
Methods/Approaches
One program was implemented for Latin America with each of the North American institutions: 1) A nephrology course about kidney transplant in 2020 with the University of Virginia (which was relaunched in English for North America in 2021); and 2) an intensive care course about end-of-life care in the ICU in 2021, with the Cleveland Clinic, which was aimed at North America and Latin America at the same time (in English, Spanish and Portuguese).
Each program averaged 25-30 hours of study over two months, and was designed as a mostly asynchronous educational intervention with social learning for massive audiences (1). Approximately 20 experts from Latin America and North America participated in each of the courses in different roles, such as coordinators, speakers, content developers and native-speaking moderators. Courses were developed in partnership with each of the two North American institutions and different academic organizations of the Latin American region, including the Brazilian Society of Intensive Care Medicine (AMIB), the Argentinean Society of Critical Care Medicine (SATI) and the Brazilian Society of Nephrology (SBN).
Each online course included study materials, in the form of texts and videos, as well as different types of activities, including discussion forums on clinical cases and clinical simulations. Simulations allowed the participant to navigate through a clinical scenario with several possible paths, where maybe more than one is correct, as in real life. Feedback is given in each step of the process. The discussion forums are virtual spaces that foster interaction with other course participants and with Faculty in their native languages (Spanish and Portuguese) The asynchronous nature of these spaces allowed the course attendees to participate whenever they could. Finally, live interactive Webinars were also part of these courses, as launching events and as synchronous conversations with the experts.
Outcomes
In the first program, (kidney transplant, 2020), there were 824 participants from 22 countries: Brazil, Mexico, Colombia, Peru, and Argentina were the top five participating countries. The second program (end-of-life care in the ICU, 2021) had 490 participants from Latin America, North America and Europe: 219 participants in the Spanish-speaking campus, 234 in the Portuguese-speaking campus and 37 in the English-speaking campus.
Regarding engagement throughout the activity, it was high along the two months in both courses despite the massive audiences. As an example, the approval requirement at the 8th week of the kidney transplant course was 60% (in this case, it was to complete a commitment to change statement). This is probably related to the social interaction among participants and with Faculty, based on social learning analytics (1).
Key Learnings for CME/CPD Practice
These programs were targeted at Interprofessional audiences with a focus on teams, and had several distinctive instructional design elements, such as being longitudinal and asynchronous/self-paced, with community and social learning, addressing massive audiences of healthcare professionals, and multilingual with a wide geographic reach. The above required collaboration to create and deliver education across languages, countries, organizations and cultures. On top of it, the pandemic created its own set of challenges and uncertainties, which necessitated flexibility and swift response in order to adapt to foreseen and unforeseen challenges.
Finally, since the educational format was new for several of the Faculty and attendees, there was a clear need for Faculty development regarding tutoring in virtual spaces, and setting up learner expectations, which also included active participation in the asynchronous conversations in order to take the most of the learning experience. 1. Margolis A, López-Arredondo A, García S et al. Social learning in large online audiences of health professionals: Improving dialogue with automated tools [version 2]. MedEdPublish 2019, 8:55 (https://doi.org/10.15694/mep.2019.000055.2)
Monitoring and Evaluating AI: Challenges and Practical Implications
Authors: Carlye Armstrong, Alexis LaCount, Alison Loughlin, Christopher Treml
Institution: American College of Radiology
Purpose/Problem Statement/Scope of Inquiry
The use of technology, particularly artificial intelligence (AI) and machine learning (ML) in medicine is currently a topic of great interest, especially with regard to diagnostic or predictive analysis of medical images. Yet AI is frequently termed a “black box” because health care professionals often have limited understanding of how it was developed and what issues may arise once AI is put into place. Health care professionals need to be empowered to use and create AI tools to meet patient needs. However, those most qualified to teach health care professionals about AI are often involved in developing AI or working with AI vendors. By integrating AI technology content into continuing education programs and recognizing the common overlap in medical professionals developing commercially available algorithms and teaching other professionals how algorithms are developed and trained CPD professionals can aim to address population health issues in the content they plan, implement and evaluate.
Approach(es)/Research Method(s)/Educational Design
Learners gained an understanding of AI terms and concepts and learned how to establish processes for vetting AI technology content into their own continuing education programs, with the ultimate aim to positively impact patient health. Learners had the opportunity to analyze case scenarios where AI may help improve care, identifying gaps/needs and learning objectives to plan a continuing education program.
Evaluation/Outcomes/Discussion
The American College of Radiology (ACR) is uniquely positioned to plan, implement and evaluate continuing education content centered on the use of AI by clinicians. The ACR’s Data Science Institute was developed to facilitate the development and implementation of artificial intelligence (AI) applications that will help radiology professionals provide improved medical care. ACR’s AI-LAB™ provides learners the ability to develop their own AI model for a specific AI use case. Learners define the problem, prepare the data, configure their own AI model and train and test the model for potential use in practice. Further, ACR hosts accredited continuing education geared at monitoring and evaluating AI in practice.
Key Learnings for CME/CPD Practice
Key learning for CME/CPD practice include: knowledge of basic AI terms, concepts and development; identification of challenges to use of AI in clinical practice; and steps to begin collaborating; and contributing to the development of AI-centered, accredited continuing education. A specific focus was placed on integrating AI technology content into continuing education programs to address population health quality gaps, with the ultimate aim to positively impact patient health based on the ACR’s experience with their continuing education program focused on AI.
Practice Assessment Tools for Medical Specialists—A Bridge to Quality Improvement
Authors: Martin Tremblay, PhD, Sam J. Daniel, MD
Institution: Federation of Medical Specialists of Quebec
Purpose/Problem Statement/Scope of Inquiry
Canada’s maintenance of certification (MOC) programs for physicians have evolved to emphasize assessment activities. Our organization has recognized the importance of providing more practice assessment opportunities for our 10,000 members to enhance their practice and help them comply with current regulations. We developed an innovative approach to structure practice-based assessments.
Approach(es)/Research Method(s)/Educational Design
Based on the Deming Cycle framework (Plan-Do-Study-Act), we developed a series of structured practice assessment documents allowing physicians to 1) determine their needs, 2) establish quality indicators, 3) analyze their practice, 4) get feedback, and 5) develop an improvement plan.
Evaluation/Outcomes/Discussion
Twenty-one practice assessment tools have been developed. They have been downloaded over 2,500 times by physicians from all 35 of our affiliated medical associations. Participants indicated that these were relevant to their practice (98%), helped them identify opportunities for improvement (97%), and prompted them to change aspect(s) of their practice (96%). These practice assessment tools are aimed at helping physicians identify knowledge or performance gaps that can be addressed with practice adjustments or further educational activities. Covering all seven CanMEDS competencies, they are intended to enable physicians claim MOC credits following various assessment activities, and unlike other assessment activities, they can be reused several times during the same MOC cycle. A collaboration with leaders from our affiliated medical associations and an efficient dissemination strategy were essential for the success of this ongoing initiative.
Key Learnings for CME/CPD Practice
Based on a quality improvement framework, we developed tools to facilitate practice assessment and identify improvement opportunities following formal and informal activities. A better integration of quality improvement principles within the discipline of CPD could improve both educational and practice-based issues.
Proactive Partnership and Project Management: A Successful Model to integrate CME into Daily Clinical Practice
Authors: Sandhya Venugopal, MD, MS-HPEd, Erik G. Laurin, MD, Shelley A. Palumbo, MS, Glee Van Loon, RD
Institution: University of California, Davis Health
Problem Statement
Education embedded in clinical practice for positive outcomes is the epitome of CME/CPD. Realizing this in a large academic medical organization, however, is not easily achieved. To effect such change, the University of California, Davis, Health Office of Continuing Medical Education (OCME) determined a multi-faceted approach built on early partnership and project management to develop quality improvement initiatives, the first of which focused on inpatient glycemic control.
Methods/Approaches
Although OCME has long been a part of quality improvement coursework, OCME needs to be involved at the ground level, ideally when gaps and needs are first identified, to effectively incorporate educational materials into daily clinical practice. To achieve this step, numerous meetings were held with leaders involved in quality initiatives across the organization, including the Chief Quality Officer. These meetings highlighted the value OCME could offer if integrated early in the process and outlined the logistics of providing educational content to address the needs.
OCME’s philosophy is that partnership is based on mutual respect and when each team member’s talents are valued regardless of their role. Everyone recognizes the value of the subject matter experts (SMEs), but equally important is the OCME team’s expertise. By welcoming OCME to develop curriculum in partnership with the Quality Office and SMEs from the outset, everyone’s expertise can be leveraged, and roles are clearly defined from the start.
The most successful projects have been those in which OCME project manages all phases of curriculum design, development, delivery, and evaluation. Project management is not to be confused with event planning, historically associated with CME. The project manager focuses on the core elements of the curriculum, leads all phases of the course lifecycle, and ensures integration into clinical practice. The inclusion of practical tools for retention and sustainability and evaluation components to measure outcomes are critical.
Outcomes
The early partnership of OCME and the quality office demonstrated the effectiveness of this model with the formation of a new inpatient glycemic control curriculum. Two learning modules were created to educate learners on ways to improve care for patients with Type 1 and 2 Diabetes Mellitus and stress-induced hyperglycemia through use of clinical decision support tools and an electronic medical record (EMR) subcutaneous insulin order set. Course content included standards of care published by the American Diabetes Association (ADA) and the application of standards into practice. Pocket reference guides were also made available for use in practice.
As a result of this CME coursework, management guidelines were updated and practice changes at an institutional level were made as demonstrated by:
- Over 1650 learners have completed the glycemic coursework to date.
- 60% of providers are now using the new Adult Subcutaneous Order Set since the launch of the two CME courses.
- The courses were highlighted during the UC Davis Health Quality and Safety Committee meeting as a Vizient Scorecard presentation under the topic of safety for reducing surgical site infections.
- A trifold of the clinical decision support tools was created as a supplement to the coursework to guide physiologic insulin in accordance with ADA standards of care for inpatient diabetes/hyperglycemia.
- Updated insulin tables now reflect coursework and order set changes within the EMR.
- Updated wording of “Adult Protocol for Insulin Infusion”
Key Learnings for CME/CPD Practice
Quality CME that permeates daily practice is possible, but several variables must be addressed to ensure success. The gaps and educational needs must be clear and have leadership support. Education must be harmonious with existing clinical processes for integration into practice. Evaluation measures identified from the beginning are critical to determine outcomes. Adjunct educational tools are beneficial for long-term sustainability. Lastly, having OCME employees with the skills to project manage these factors is essential.
The utilization of a CME project management model facilitates best practice and ensures curriculum is developed in a manner that includes multiple integrative elements. By applying this approach, it is possible to incorporate education into daily practice. While project management is not a new concept, it is not widely applied in CME/CPD. Given the clear benefits, this approach may be considered for initiatives requiring widespread change.
Developing a Patient Safety Culture Training Curriculum for Healthcare Professionals
Authors: Eulaine Ma, BSc, Wei Wei, BSc, Certina Ho, BScPhm, PhD
Institution: Leslie Dan Faculty of Pharmacy, University of Toronto
Purpose/Problem Statement/Scope of Inquiry
The Patient Safety Reporting and Learning (PSRL) Committee of the Manitoba Institute for Patient Safety (which is now under Shared Health’s Quality and Learning service in Manitoba, Canada) was committed to develop a community-based incident reporting and learning system for multi-disciplinary healthcare professionals in Manitoba. The PSRL Committee was fully aware that building and nurturing safety culture among all health professions was a prerequisite for developing and maintaining an effective patient safety incident reporting and learning system. Lessons learned from other reporting and learning systems around the world reflected that low reporting and utilization rates of such programs were associated with poor safety culture. On the other hand, having a patient safety culture is a facilitator for incident reporting and learning.
Patient safety culture is defined as the shared organizational belief and behavioural pattern that focuses on maximizing patient safety and minimizing patient harm. It is a key component of enhancing patient safety, and therefore quality of care. As well, establishing and maintaining a patient safety culture is an indispensable prerequisite for an organization or a regulatory authority to implement any patient safety and quality improvement initiatives.
The purpose of our project was to identify existing patient safety culture education guiding documents, synthesize these materials, and develop a specific curriculum for training healthcare professionals on safety culture. Ultimately, this patient safety culture curriculum will not only support a multi-disciplinary provincial regulatory authority (e.g., in Manitoba, Canada) in advocating for patient safety culture and province-wide quality improvement initiatives, but also aid in establishing or improving safety culture in any organization.
Approach(es)/Research Method(s)/Educational Design
A formal literature search on MEDLINE® and EMBASE was performed for training materials specific to patient safety culture but did not return any results that the PSRL Committee and patient safety stakeholders could readily use or apply to meet their needs in Manitoba. Thus, we discovered that there is a paucity of ready-to-use and translatable patient safety culture training materials in the literature for regulatory or health professional bodies to apply across a multi-disciplinary healthcare setting.
We then performed a grey literature search to find relevant guiding documents from patient safety organizations, including those in the United Kingdom (UK), Canada, United States (US), Australia, New Zealand, and the World Health Organization (WHO), all of which have either similar health systems or established patient safety organizations or efforts. To identify websites of regulatory authorities and policy institutes responsible for patient safety, we used a simple Google search, then located relevant documents on these sites via targeted Google search. This involved using Google search queries related to patient safety that were restricted to a particular organization’s website.
To synthesize the patient safety culture curriculum, individual domains, competencies, or relevant themes from our identified patient safety education guiding documents were compared and overlapping competencies relevant to patient safety culture were extracted. Common patient safety culture topics were constructed into a curriculum using Bloom’s taxonomy and the Knowledge, Skills, Attitude learning outcome categories. (Figure 1 – link to Safety Culture Curriculum Syllabus for HCPs 18Feb2022.PDF)
Evaluation/Outcomes/Discussion
Four patient safety education guiding documents were identified. These documents were National Patient Safety Syllabus 1.0 (National Health Service, 2020), The Safety Competencies (Canadian Patient Safety Institute, 2020), Safer Together: A National Action Plan to Advance Patient Safety (Institute for Healthcare Improvement, 2020), and the Patient Safety Curriculum Guide (Multi-professional Edition) (WHO, 2011). The curriculum was synthesized with a total of five competencies and 21 learning objectives. The five competencies are organizational culture, just culture, safety improvement and evaluation, information sharing and transparency, and safety leadership. (Figure 1)
Organizational culture and just culture address barriers and facilitators to reporting safety incidents. Regarding organizational culture, including patient safety in an organization’s values or vision encourages engagement from staff and facilitates incident reporting. A just culture is about approaching errors from a system perspective rather than blaming and shaming individuals involved, which can remove a significant barrier for reporting. Both themes help set the tone for safety culture from a bottom-up perspective within a workplace or practice setting.
A top-down perspective is related to safety leadership. Safety leaders promote safety culture through leading by example and inspiring others to appreciate the value of patient safety culture. They also oversee and reinforce the organizational culture and just culture, our last two competencies, by facilitating the use of quality improvement and reporting tools. Safety leadership also has a bottom-up contribution, where safety leaders empower healthcare providers within a team to be safety leaders themselves, promoting safety culture and engaging colleagues to embrace and uphold organizational and just culture, the first two competencies.
Safety improvement and evaluation highlights the need to measure patient safety through enabling healthcare providers, patients, and families to report and share safety incidents. These incidents should also be appropriately evaluated and analyzed to determine root causes, contributing factors, and areas of improvement. Information sharing and transparency is a related, but separate competency that emphasizes the importance of closing the loop on reported incidents, which can be done through analysis and dissemination of shared learnings. Both themes can be addressed simultaneously with continuous quality improvement initiatives supported by an accessible, user-friendly, and well received/used patient safety incident reporting and learning system.
Key Learnings for CME/CPD Practice
The Safety Culture Curriculum for Health Care Professionals (Figure 1) serves as a step forward in creating ready-to-use and translatable patient safety culture training materials for healthcare providers. It can be used to develop educational or training modules specific to any levels within an organization, including teams, institutions, or jurisdictions. All five competencies should be addressed in a patient safety culture curriculum, which can be further guided by the learning objectives suggested within each competency domain (Figure 1).
The topic of patient safety culture, although often explored in undergraduate training for medical and healthcare professions, continue to be significant and relevant when one begins their clinical practice with direct patient care. Therefore, patient safety culture training is well suited for CME/CPD for healthcare practitioners. Potential next steps of the Safety Culture Curriculum for Health Care Professionals (Figure 1) include content creation, development, and delivery of materials, such as training courses, modules, workshops, or seminars, etc., which can be pilot tested virtually and/or locally at targeted sites or jurisdictions to obtain feedback and lessons learned. Specific learning objectives may also be adapted and integrated into existing “in-house” patient safety training programs at different institutions, to provide insights on how the curriculum may be operationalized in real-world healthcare settings. The cultural context of a practice setting has an impact on the practice of a healthcare provider or a team, and subsequently the quality and safety of patient care. The myriad of educational sessions organized by local CME/CPD programs offer great opportunities for CME/CPD providers to utilize or adapt the curriculum in an innovative and customized manner, as part of a concerted effort to build and promote patient safety culture in the workplace. The Safety Culture Curriculum for Health Care Professionals (Figure 1) may serve as a primer for further education and research in patient safety culture, as greater inclusion of human and system factors that affect patient care in CME/CPD programs is warranted.
Impact of Interprofessional vs Non-interprofessional Continuing Education Activities on Learning, Competence, and Performance Pertaining to Interprofessional Collaborative Practice
Authors: Marianna Shershneva, MD, PhD, Barbara Anderson, MS
Institution: Office of Continuing Professional Development, University of Wisconsin School of Medicine and Public Health
Purpose/Problem Statement/Scope of Inquiry
The University of Wisconsin-Madison Interprofessional Continuing Education Partnership (ICEP) conducts an annual survey of participants in the ICEP-accredited activities. Analysis of responses to open-ended questions about the educational impact from the 2016-2020 surveys documented that reported changes in competence and performance resulting from participation in interprofessional (IP) as well as non-interprofessional (non-IP) activities included statements consistent with collaborative practice. This observation and a transition from open-ended to multiple choice survey questions pertaining to the educational impact created an opportunity to examine outcomes from IP activities in comparison with non-IP activities. We used the results of the 2021 survey to answer two questions. Did non-IP activities have impact in areas consistent with IP, collaborative practice? Was this impact comparable to the impact of IP activities? Moore’s levels of evaluation and four domains of IP practice informed our inquiry.
Approach(es)/Research Method(s)/Educational Design
The survey included blocks of questions about live, enduring, and regularly scheduled series (RSS) activities. Respondents could select one activity they participated in (or none) from a list in each block, and then evaluate the selected activity by responding to the related questions. We analyzed responses to the following questions:
- Did participation in this activity impact your knowledge, attitudes, and/or skills/strategy/ability to act pertaining to your practice?
- Those who answered “yes”, were asked: How did you change your knowledge, attitudes, and/or skills/ability to act? Respondents could select all that applied; 4 of 12 listed categories pertained to IP practice.
- Did participation in this activity impact your and/or your healthcare team performance/practice?
- Those who responded “yes”, were asked: How did you and/or your healthcare team improve performance/practice? Respondents could select all that applied; 2 of 18 listed categories pertained to IP practice.
Responses pertaining to domains of IP practice were compared for IP activities vs non-IP activities using Fisher exact test with significance level P<0.05.
Evaluation/Outcomes/Discussion
A total of 602 education participants representing more than 20 professions responded to the survey. Distribution by profession is shown in Figure 1 below.
Results for IP activities vs non-IP activities responses were as follows. Education impacted learning and competence: 89% of 341 respondents vs 91% of 127 respondents. Education impacted performance: 76% of 311 respondents vs 72% of 128 respondents. Those who reported impact specified changes by listed categories (Table 1 and Table 2). Applying values/ethics to IP practice: knowledge 52% vs 48%, attitude 14% vs 11%, competence 30% vs 23%. Communication with other professionals: knowledge 45% vs 40%, attitude 13% vs 9%, competence 32% vs 27%. Defining the roles/responsibilities: knowledge 44% vs 35%, attitude 14% vs 13%, competence 25% vs 24%. Working with an IP team: knowledge 44% vs 39%, attitude 15% vs 13%, competence 26% vs 23%. Collaboration between team members: learner performance 42% vs 38%, team performance 41% vs 29%. Communication with other healthcare professionals: learner performance 44% vs 35%, team performance 38% vs 29%. None of the comparisons showed a significant difference.
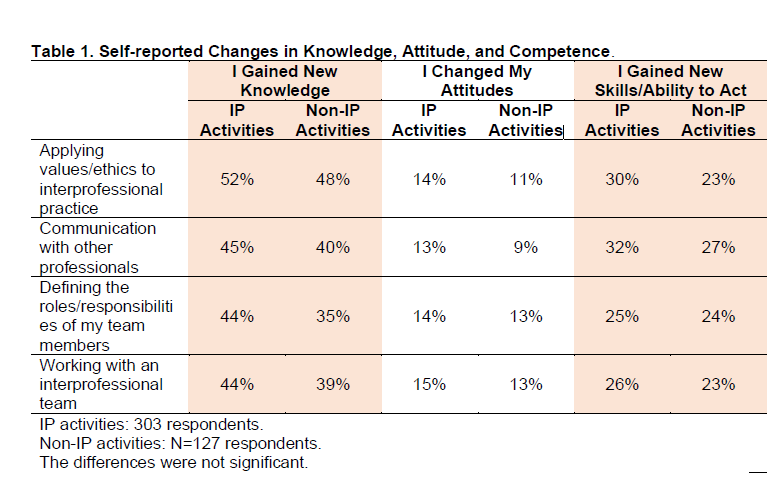
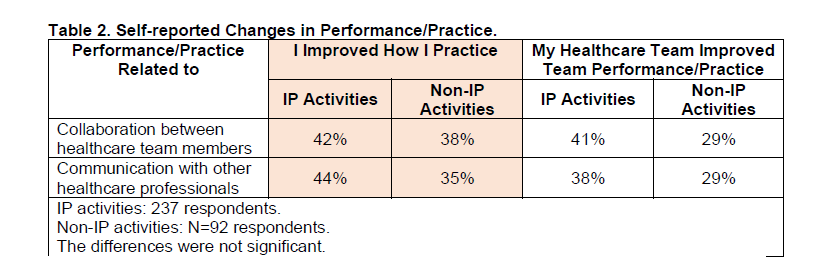
Key Learnings for CME/CPD Practice
All activities in our evaluation study had impact in the areas pertaining to IP practice, with no significant differences between IP and non-IP activities. Published studies comparing outcomes between IP and uniprofessional education of clinicians or clinicians-in-training show mixed results. For example, in a study conducted in the United Kingdom, nurses/midwives and foundation year doctors were assigned to either IP or uniprofessional groups to participate in a one-day simulation course. IP groups were associated with better outcomes for communication and teamwork.[1] Similarly, another European study showed better outcomes for communication and teamwork skills resulting from an IP course on diabetes for students of medicine, dentistry and nursing vs from the same education done as a uniprofessional course [2]. However, in a Korean study, an IP group of medical and nursing students and auniprofessional group of medical students participated in a class on team communication and IP collaboration; outcomes were measured by Interprofessional Attitudes Scale (IPAS) and the Self-Efficacy Perception for Interprofessional Experiential Learning (SEIEL) scale and were similar for both groups [3].
Intentional effort to change institutional culture towards embracing IP values may explain documented impact of IP and non-IP activities in our program. Additionally, employing our continuing education planning process that is supportive of collaborative, IP learning could influence the educational design and delivery of uniprofessional education for learners as members of the healthcare team, leading to the observed outcomes.
The results of our study could not be generalized to other settings, and educational strategies used in the evaluated activities were not considered in the analysis. Other limitations include self-reported data with a possibility of poor recall or social desirability bias. Future research is needed to explore how and why learning experience and resulting outcomes differ between IP and non-IP continuing education for healthcare professionals.
References
1. Watters C, Reedy G, Ross A, Morgan NJ, Handslip R, Jaye P. Does interprofessional simulation increase self-efficacy: a comparative study. BMJ Open. 2015;13;5(1):e005472. doi: 10.1136/bmjopen-2014-005472. PMID: 25586366; PMCID: PMC4298099.
2. Račić M, Joksimović BN, Cicmil S, et al. The effects of interprofessional diabetes education on the knowledge of medical, dentistry and nursing students. Acta Med Acad. 2017;46(2):145-154. doi: 10.5644/ama2006-124.199. PMID: 29338278.
3. Park YC, Park KH. Interprofessional education program for medical and nursing students: interprofessional versus uniprofessional. Korean J Med Educ. 2021;33(1):1-10. doi: 10.3946/kjme.2021.182. Epub 2021 Mar 2. PMID: 33735552; PMCID: PMC7973076.
Preparing Physicians to Lead Organizational Change
Authors: Jessica L. Walter, EdD, MA
Institution: Rossier School of Education, University of Southern California
Purpose/Problem Statement/Scope of Inquiry
As hospitals seek to increase physician executives (Robeznieks, 2014), physicians may not be prepared to assume these responsibilities and roles (Angood & Birk, 2014; Steinert et al., 2012). Healthcare systems and hospitals are complex (Coiera, 2011; Lavoie et al., 2017; Stoller et al., 2016). Not only have good management and leadership been linked to positive hospital outcomes (Bloom et al., 2012; Gupta, 2019), but they are imperative for healthcare systems to reach their goals (Bloom et al., 2014; Stevenson & Moore, 2018). Therefore, it is not surprising that physicians are continuing their education (Turner et al., 2018). Continuing medical education (CME) and graduate education are two vehicles for physicians to close gaps in leadership skills. CME offerings lack content to develop leadership skills and evaluation thereof (Kitto et al., 2013). While these skills are considered important, they are not well defined in this population (Balmer, 2013) and are difficult to measure and assess (Allen et al., 2019). Alternatively, graduate business education may assess classroom-based learning associated with management skills, but the content may not be tailored to healthcare professionals nor routinely explore how students apply their education to the workplace. This program evaluation explored how physicians enrolled in a healthcare-specific MBA program transferred knowledge from a health systems course, for which they earned CME credit, to their workplaces. Furthermore, awarding CME for graduate coursework is a novel concept. The study explored knowledge retention, physicians' motivations to implement recommendations, and perceived barriers and facilitators to change.
Approach(es)/Research Method(s)/Educational Design
Educational Design The educational design for the course was grounded in the transformative model. The transformative model asks learners to connect what they learn to their everyday lives (Lazowski & Hulleman, 2016). In addition to asynchronous forum posts, where learners explored weekly concepts and exchanged ideas, each student wrote a consulting report analyzing their organization through the lens of the Quadruple Aim (Bodenheimer & Sinsky, 2014). They gathered primary and secondary data, conducted a gap analysis (Clark & Estes, 2008), and ultimately created recommendations for their organization, including proposals upon which they could act. Conceptual Model Bandura's social cognitive theory (1986) formed the foundation of the conceptual model. This tripartite model, describes the mutual influences of the person's inner world (knowledge and motivational factors), their environment (workplace culture and policies, education setting), and their behavior (commitment to change, progress toward goals, perceived barriers and facilitators). Study Design In this qualitative study, each participant completed a 90-minute interview. The interview consisted of structured questions to assess knowledge recall, self-efficacy, and progress toward goals. These took place via video conferencing. Open-ended questions further assessed motivation and environmental factors (workplace, education). Questions assessing self-efficacy were developed using Bandura's protocols (Bandura, 2006), while knowledge, motivation, and queries about their environments were derived from the study questions. Knowledge retention and ratings of self-efficacy were enumerated; interviews were coded using thematic analysis (Gibbs, 2018). Participants Five (56%) physicians completed the interview of the nine invited to participate. Non-physicians and physicians who did not claim CME were not invited. All were working along the West Coast, representing rural and urban settings; they had an average of 20 years of professional practice.
Evaluation/Outcomes/Discussion
Physicians transferred their learning from their coursework into their workplace with varying degrees of success. Physicians recalled key concepts and rated themselves as self-efficacious in using knowledge to make system-level changes. However, physicians struggled to implement change beyond their individual practice, citing personal and workplace factors.
Physicians accurately recalled the four aims of the Quadruple Aim (Bodenheimer & Sinsky, 2014); however, they struggled to recall the aspects of the gap analysis (Clark & Estes, 2008). This difference may be because they had previous, repeated exposure to the Quadruple Aim, where the gap analysis was a new framework and one in which they did not have much guided learning.
Physicians were motivated to make changes in their workplace. They consistently spoke of improving the system for their peers and patients. They expressed strong self-efficacy in applying both the Quadruple Aim and the gap analysis to achieve their goals even as they struggled to recall key elements of the gap analysis. Their self-efficacy may stem from having made progress toward their goals over the intervening months and their continued desire to see progress. Only one physician said he would not continue to work on their goals, citing changes in the workplace and the subsequent need to set new goals.
Furthermore, physicians were more likely to make progress on goals within their personal practice than within the larger system. One physician answered questions twice, once as a practicing physician and again as a board member for his region's accountable care organization. He specifically noted the challenges associated with larger-scale change.
Physicians found success in creating change when their goals aligned with organizational goals or were supported by the organization. They were more successful in changes where they had decisional control and felt knowledgeable. Changes beyond their own practice benefited from leadership support, formal leaders (who assigned authority and resources) and informal mentors. Furthermore, they saw interdisciplinary teamwork as instrumental to larger-scale improvements but worried about infringing on the practice of other physicians. Detractors from success included system complexity, a lack of access to decision-makers, individualism or heroics, competing priorities, and change fatigue. They recognized that external factors influenced their organizations and, therefore, their projects, especially shifting regulation, the political uncertainty following the 2020 U.S. presidential election, and with COVID-19.
This study revealed several areas for improvements to the education environment. First, faculty can increase the use of spaced learning and scaffolding when applying the gap analysis to the four aims. Spaced learning improves knowledge acquisition (Agarwal & Bain, 2019; Berrett-Abebe et al., 2019; Flett et al., 2018; Gooding et al., 2017) and allows for targeted feedback (Ambrose et al., 2010). Second, physicians noted that they had not previously learned to write for a business audience and may not have seen many examples. Providing more structure and resources for interviewing leaders, formatting their analysis, and creating recommendations could help physicians make more actionable goals. By incorporating the facilitators and barriers physicians experience into the education environment, course developers can help learners create more achievable goals. Finally, physicians wanted to hear from others who have led successful change, a form of vicarious modeling (Bandura, 1997). Taken together, these changes position the course to increase the transfer of learning and working toward system improvements.
Key Learnings for CME/CPD Practice
- Physicians have a strong desire to improve the healthcare system for patients and peers.
- Physicians need more exposure to and guided practice in applying systems thinking frameworks.
- Course developers can help physicians improve their recommendations through structured processes that encourage learners to link their recommendations with organizational goals.
- The education environment can encourage learners to explore competing priorities and complexities of the system when conducting their analysis.
- This program evaluation provided insights for a specific experience and audience. The transferability of the information, therefore, is limited. However, there may be transferability to future collaboration between CME and degree-awarding programs.
References
Agarwal, P. K., & Bain, P. M. (2019). Powerful teaching: Unleash the science of learning. John Wiley & Sons.
Allen, L. M., Palermo, C., Armstrong, E., & Hay, M. (2019). Categorising the broad impacts of continuing professional development: A scoping review. Medical Education, 53(11), 1087–1099. https://doi.org/10.1111/medu.13922
Ambrose, S. A., Bridges, M. W., DiPietro, M., Lovett, M. C., & Norman, M. K. (2010). How learning works: Seven research-based principles for smart teaching. John Wiley & Sons.
Angood, P., & Birk, S. (2014). The value of physician leadership. Physician Executive, 40(3), 6.
Balmer, J. T. (2013). The transformation of continuing medical education (CME) in the United States. Advances in Medical Education and Practice, 4, 171–182. PubMed. https://doi.org/10.2147/AMEP.S35087
Bandura, A. (1986). Social foundations of thought & action: A social cognitive theory. Prentice-Hall.
Bandura, A. (1997). Self-Efficacy: The exercise of control. Freeman.
Bandura, A. (2006). Self-efficacy beliefs of adolescents. Guide for Constructing Self-Efficacy Scales, 5, 307–337.
Berrett-Abebe, J., Cadet, T., Nekhlyudov, L., Vitello, J., & Maramaldi, P. (2019). Impact of an Interprofessional Primary Care Training on Fear of Cancer Recurrence on Clinicians’ Knowledge, Self-Efficacy, Anticipated Practice Behaviors, and Attitudes Toward Survivorship Care. Journal of Cancer Education, 34(3), 505–511. https://doi.org/10.1007/s13187-018-1331-y
Bloom, N., Sadun, R., & Reenen, J. V. (2012). Does Management really work? Harvard Business Review, November. https://hbr.org/2012/11/does-management-really-work
Bloom, N., Sadun, R., & Van Reenen, J. (2014). Does management matter in healthcare. Boston, MA: Center for Economic Performance and Harvard Business School.
Bodenheimer, T., & Sinsky, C. (2014). From Triple to Quadruple Aim: Care of the patient requires care of the provider. The Annals of Family Medicine, 12(6), 573–576. https://doi.org/10.1370/afm.1713
Clark, R. E., & Estes, F. (2008). Turning research into results: A guide to selecting the right performance solutions. IAP.
Coiera, E. (2011). Why system inertia makes health reform so difficult. BMJ, 342. https://doi.org/10.1136/bmj.d3693
Flett, K. B., Bousvaros, A., Carpenter, J., Millrinen, C. E., Martin, P., & Sandora, T. J. (2018). Reducing Redundant Anaerobic Therapy Through Spaced Education and Antimicrobial Stewardship Interventions. Journal of the Pediatric Infectious Diseases Society, 7(4), 317–322. https://doi.org/10.1093/jpids/pix090
Gibbs, G. R. (2018). Analyzing qualitative data (Vol. 6). Sage.
Gooding, H. C., Cheever, E., Forman, S. F., Hatoun, J., Jooma, F., Touloumtzis, C., & Vernacchio, L. (2017). Implementation and evaluation of two educational strategies to improve screening for eating disorders in pediatric primary care. Journal of Adolescent Health, 60(5), 606–611. https://doi.org/10.1016/j.jadohealth.2016.12.002
Gupta, A. K. (2019). Physician versus non-physician CEOs: The effect of a leader’s professional background on the quality of hospital management and health care. Journal of Hospital Administration, 8(5).
Kitto, S., Bell, M., Goldman, J., Peller, J., Silver, I., Sargeant, J., & Reeves, S. (2013). (Mis)perceptions of Continuing Education: Insights From Knowledge Translation, Quality Improvement, and Patient Safety Leaders. Journal of Continuing Education in the Health Professions, 33(2), 81–88. https://doi.org/10.1002/chp.21169
Lavoie, K. L., Rash, J. A., & Campbell, T. S. (2017). Changing Provider Behavior in the Context of Chronic Disease Management: Focus on Clinical Inertia. Annual Review of Pharmacology and Toxicology, 57(1), 263–283. https://doi.org/10.1146/annurev-pharmtox-010716-104952
Lazowski, R. A., & Hulleman, C. S. (2016). Motivation Interventions in Education: A Meta-Analytic Review. Review of Educational Research, 86(2), 602–640. https://doi.org/10.3102/0034654315617832
Robeznieks, A. (2014, May 10). Hospitals hire more doctors as CEOs as focus on quality grows. Modern Healthcare. https://www.modernhealthcare.com/article/20140510/MAGAZINE/305109988/hospitals-hire-more-doctors-as-ceos-as-focus-on-quality-grows
Steinert, Y., Naismith, L., & Mann, K. (2012). Faculty development initiatives designed to promote leadership in medical education. A BEME systematic review: BEME Guide No. 19. Medical Teacher, 34(6), 483–503. https://doi.org/10.3109/0142159X.2012.680937
Stevenson, R., & Moore, D. E. (2018). Ascent to the summit of the CME pyramid: Defining outcomes for CME activity. JAMA, 319(6), 543–544. https://doi.org/10.1001/jama.2017.19791
Stoller, J. K., Goodall, A., & Baker, A. (2016, December 27). Why the best hospitals are managed by doctors. Harvard Business Review. https://hbr.org/2016/12/why-the-best-hospitals-are-managed-by-doctors
Turner, A. D., Stawicki, S. P., & Guo, W. A. (2018). Competitive advantage of MBA for physician executives: A systematic literature review. World Journal of Surgery, 42(6), 1655–1665. https://doi.org/10.1007/s00268-017-4370-3
The Role of Regulators and Professional Regulations in Fostering the Use of Electronic Health Data to Strengthen Continuing Professional Development (CPD) for Medical Practitioners. A Documentary Data Analysis and Semi-Structured Interviews with Key Informants
Authors: Carol Pizzuti, MRes Medical Anthropology, Dr. Cristiana Palmieri, PhD, Prof. Tim Shaw, PhD
Institutions: The University of Sydney, The Digital Health CRC, The Royal Australasian College of Physicians (RACP)
Purpose/Problem Statement/Scope of Inquiry
There is growing interest in strengthening CPD for medical practitioners in the Australasian context. Along with other principles, Australasian medical regulatory bodies have stated that CPD programs must be aligned to the practitioner’s scope of practice and interrelated to quality care and patient safety. For this reason, great emphasis has recently been placed on CPD activities that aim at reviewing performance and measuring health outcomes.
Health data analysis for performance feedback is at the core of those CPD activities. Unfortunately, the literature suggests that many of these work-based CPD activities – such as Audit and Feedback (A&F) interventions, Quality Improvement (QI) projects, and other performance measure initiatives – are still reliant on manual data collection, analysis, and reporting.
Electronic health data analytics and visual analytics tools serve as a digital solution to simplify these tasks and streamline processes, making the completion of these activities less lengthy and burdensome for medical practitioners.
Despite the current shift in CPD requirements for medical practitioners and the need to improve health data analysis practices for CPD purposes, there is lack of awareness in relation to medical regulators’ standpoints and policy implementation strategies to foster the use of electronic health data analytics technologies.
This study aims to fill this research gap, focusing on the analysis of existing regulatory policies for medical practitioners in 5 selected countries and collecting the opinions and insights of international key informant in the field. Specifically, this study intends to clarify: a) which CPD categories and CPD activities need the use of health data to be completed; b); if CPD requirements explicitly suggest and/or mandate the use of electronic health data for the completion of these activities; c) how medical regulators envision the use of electronic health data for performance feedback and strengthened CPD in the near future; and d) what role medical regulators are willing to play in order to foster the use of electronic health data analytics for CPD purposes.
Approach(es)/Research Method(s)/Educational Design
As a first step, an environmental scan was conducted to identify relevant Medical Regulatory Bodies in Australia, Canada, New Zealand, the UK, and the US. Subsequently, relevant policies and other documentary data on medical regulations and CPD requirements developed by these bodies were identified and stored in NVivo.
All the collected documents are currently under analysis in order to review and examine content and aims. The analysis is being undertaken using the “READ” approach, which consists of 4 steps: 1. Ready your materials; 2. Extract data; 3. Analyse data; and 4. Distil your findings.1
Document analysis is a systematic procedure for reviewing or evaluating documents, and its results are often triangulated with interviews and other sources of data, such as academic literature.2 For this study, semi-structured interviews with key informants in the field were conducted in order to cross-validate findings and deepen the insights of the documentary data analysis.
Regarding the method employed to conduct the interviews, research participants were identified during the environmental scan. 28 bodies were invited to participate in the study via email. 13 different regulatory bodies agreed to contribute to the research study, for a total of 20 key informants.
Interviews were conducted on Zoom, following a pre-approved semi-structured outline. Audio- and video-recordings of all interviews were stored on university-supported digital tools and platforms, and audio-recordings were transcribed using Descript.
All the interview transcriptions were then stored in NVivo, and they are currently being analysed using the Braun and Clarke’s contemporary approach to reflexive thematic analysis3 to investigate: a) context, rationale, and applicability of medical regulations; and b) standpoint of medical regulators with regard to the potential use of electronic health data analysis for CPD purposes and their role in such endeavour.
Evaluation/Outcomes/Discussion
An initial analysis of the documentary data confirms a relatively recent shift in medical regulations and CPD requirements in all the countries under investigation. Depending on the jurisdiction, over the last 10 to 20 years medical regulators have in fact placed more emphasis on those CPD activities that aim at reviewing clinical performance using patient-related data analysis.
Despite this conceptual shift in regulatory policies, very few CPD frameworks and programs mention the use of electronic health data for such purposes. According to many key informants, the reason behind this choice mainly lies on the broad meaning that many medical regulators give to the concept of data for performance feedback. In addition to this, most regulators reported that the use of electronic health data is not explicitly recommended nor deemed as compulsory due to the existence of major data accessibility issues in the healthcare system. In fact, it has been reported that the necessary health data is not always readily available to the practitioner or, if available, it is often manually collected, analysed, and reported. Moreover, some informants shared that in their jurisdiction – or specific parts of it – patient health data analysis is still reliant on paper-based charts and supporting documents.
As a final remark, most participants indicated that regulatory bodies do not have the responsibility nor the power to address the abovementioned issues, considering that health data collection, analysis, and reporting is in the hands of health-care service organizations.
Given this, several informants pointed out that the only barriers that can be addressed by the regulators are the following:
Data accessibility issues, and only through advocacy and lobbying.
Lack of workforce capabilities with regards to data collection, analysis, reporting, interpretation, and actionability. Such role has been mentioned especially by those bodies that set CPD requirements and also offer and deliver CPD programs and activities.
Further research on the topic, especially through active collaboration and partnership with commercial and industry groups, with the ultimate aim of starting to imagine the future and planning strategies for technology design and implementation.
If electronic health data analysis has to be used to strengthen CPD, many barriers and challenges will need to be addressed first, and regulatory bodies have limited power in this regard. Nonetheless, they have shown great interest in the use of data analytics for CPD purposes, and they recognize the value of this new field of research.
Key Learnings for CME/CPD Practice
Study results are expected to support medical regulatory and certifying bodies in their efforts to foster data-strengthened CPD.
Ideally, final research considerations will promote the development of clear policy implementation strategies and encourage the design and utilisation of the digital technologies and tools for data driven CPD programming and planning.
References
1 Dalglish, S. L., Khalid, H. and McMahon, S. A. (2020) ‘Document analysis in health policy research: The READ approach’, Health Policy and Planning, 35(10), pp. 1424–1431. doi: 10.1093/heapol/czaa064.
2 Gross, J. M. S. (2018) ‘Document analysis’, in Frey, B. B. (ed.) The SAGE Encyclopedia of Educational Research, Measurement, and Evaluation. Thousand Oaks, CA: SAGE Publications, Inc., pp. 545–548. doi: 10.4135/9781506326139.
3 Braun, V. and Clarke, V. (2006) ‘Using thematic analysis in psychology’, Qualitative Research in Psychology, 3(2), pp. 77–101. doi: 10.1191/1478088706qp063oa.
Back To TopInnovating and Adapting in Changing Times
A Call to Action: Committing to Diversity, Equity, and Inclusion in CPD
Author: Annette Donawa, PhD
Institution: Thomas Jefferson University School of Medicine, Office of Continuing Professional Development
Purpose/Problem Statement/Scope of Inquiry
Thomas Jefferson Office of Continuing Professional Development (OCPD) is committed to expanding Diversity, Equity, and Inclusion efforts pertaining to CPD. This call to action to create a DEI strategic plan began in 2020 when the mission and vision statements were revised to reflect inclusion language to support Jefferson’s overall mission.
Theoretical Framework
Brainstorming and feedback sessions held with leadership and OCPD staff to examine the expansion of DEI initiatives in CPD. Brainstorming, reflections, and peer feedback on recommendations guided the DEI strategic plan.
Methods/Approach
Brainstorming and feedback sessions with leadership and staff for six months led to the initial DEI strategic plan:
1. Phase 1: Include DEI language in mission and vision statements
2. Phase 2: Include health equity language to the Continuing Education (CE) Application
3. Phase 3: Partner with the institution’s DEI office to accredit courses (non-clinical topics)
4. Phase 4: Include questions on the CE Application to include diverse perspectives from speakers and topic selections
5. Phase 5: Create annual CPD award recognizing departments that models inclusion of DEI.
Findings/discussion
Jefferson leadership and OCPD embrace DEI initiatives and responded positively to brainstorming and making recommendations on expanding DEI in CPD. Highlighting model departments in this effort will further support the DEI strategic plan.
Impact/relevance to the advancement of the field of CME/CPD
CPD offices nationally and globally can make a positive impact on expanding DEI. Strategically positioning these offices in the ‘driver’s’ seat can make a difference within their respective institutions. Being bold and brave to change the DEI landscape by developing a DEI strategic plan is a noteworthy call to action.
CPD Diversity Audit: Tracking and Reflecting on CPD Decisions for Advancing Justice
Authors: Eleftherios Soleas PhD, Tiffany Mak MPH, Katherine Evans BA, Jenny DeBruyn BA, Mikaila De Sousa PME, Kate Kittner BA, and Richard van Wylick MD
Purpose
Representation matters in teaching and learning. This is true also in CPD where who is chosen to present a topic reflects who is seen as knowledgeable and spotlighted. At Queen’s, the advancement of justice through equity, diversity, inclusion, and indigeneity is a priority. We decided to put our money where our mouth is and see what a years’ worth of effort in deliberately seeking representative planning committees in profession, racialized, and other equity-deserving groups would do for the representativeness and contextual representativeness of the CPD offerings that our office produced.
Approach
We integrated resources such as Visual Dx as well as enhanced guidelines for speakers approved by our planning committees which prompted for more representativeness in the creation of educational materials such as slides, quizzes, modules, and pictorial representations of signs, symptoms, and patients. We retrospectively performed a content analysis of our 2019 and 2020 CPD offerings to see the extent that our planning committees and educational materials in our programs reflected the diversity of Canadian healthcare. We applied our learning and new procedures to our 2021 offerings and going forward.
Outcomes and Discussion
We integrated resources such as Visual Dx as well as enhanced guidelines for speakers approved by our planning committees which prompted for more representativeness in the creation of educational materials such as slides, quizzes, modules, and pictorial representations of signs, symptoms, and patients. We retrospectively performed a content analysis of our 2019 and 2020 CPD offerings to see the extent that our planning committees and educational materials in our programs reflected the diversity of Canadian healthcare. We applied our learning and new procedures to our 2021 offerings and going forward.
Key Learnings for CME/CPD Practice
1. Providing resources for planning committees and speakers as well as clear expectations creates the right mix of support and guidance to propel change
2. This change, like many others, depends on the will to follow through. It is far too easy to slip back into old patterns and behaviours that led to this type of intervention being necessary
3. The continued acquisition and creation of resources to include in communications with planning committees and speakers is vital
It’s a Dog’s World: Leveraging Veterinary Education Lessons and Experience in Launching an Accredited CE Program
Authors: Taylor Webb MPH, Shawna Clawson OTR/L, Shawn Tsuda MD, Renea Marin CHCP, Aubrey Arreola, Paula Deal
Institution: Viticus Group
Purpose
In 1997 the American Association of Veterinary State Boards (AAVSB) established the Registry of Approved Continuing Education (RACE) to establish uniform standards for providing CE to veterinary professionals. Viticus Group (VG), a 501 (c)(3) organization with two facilities in Las Vegas, NV, totaling over 140,000 sq ft facility, has been providing RACE approved CE hours for many years. In December of 2020, VG obtained ACCME accreditation, leveraging its veterinary resources and experience to institute a continue medical education (CME) program-Viticus Academy, to expand the impact VG has on CE for the healthcare team.
Approaches
In order to create a new human health education division enterprise level resource allocation involving financial, physical, and human technological components was necessary. As an organizational strategy, VG looked to add human CME activities to the existing veterinary CE program through functional, divisional, and a combined organizational structure. As a result, we utilized a functional structure of existing business divisions including operations, marketing, finance, and IT to organize two pre-accreditation (internet enduring activities) and plan two post-accreditation (one live didactic course and one internet enduring) CME activities for the inaugural year in the topic area of COVID-19. VG looks to leverage this model for expansion into a well-designed, high-impact program with continued effort on high-quality and evidence-based educational opportunities, for not only physicians, but the entire healthcare team.
Discussion
CME activities at VG benefitted from shared veterinary CE resources and experience, though initial low attendance suggests practice gap analysis and marketing may require transition to a divisional structure with dedicated CME resources. High participant evaluation scores, however, demonstrated the effectiveness of leveraged resources in the areas of content-creation, speaker effectiveness, and compliance. These high scores included 100% strong agreement when asked if the teaching and learning methods were effective.
Viticus Group’s history of providing veterinary CE assisted the new human CME division primarily by utilizing the same methodology for certain processes. These processes included sending front matter to participants, creating post course surveys, and conducting needs assessments. However, there were several stark differences that VG had to adapt to. The first difference is that the veterinary CE program has been developed over many years and has an extensive data base for both speakers and participants. With 2021 being the inaugural year of Viticus Academy it was starting from scratch with no database of pre-screened speakers to leverage, coupled with developing an entire program in a global pandemic. Secondly, the veterinary CE program has much more funding as there are little to no regulations regarding sponsorship/vendors and their long-standing brand recognition draws sponsors to them. Finally, VG hosts one of the largest veterinary conferences worldwide which is full of opportunities for attendees to earn CE credits. The veterinary CE program’s ability to provide these credit opportunities is largely due to their rules and regulations being much less stringent than the ACCME.
Key Learnings for CME/CPD Practice
Viticus Group’s mission to provide education to both veterinary and human health professionals is relevant as free-standing and university affiliated hands-on procedural institutes often share resources with veterinary education counterparts. Additionally, the sharing of resources and collaboration between our veterinary CE program and accredited-CME program is another step towards the actualization of the One Health Initiative. Utilizing a combined structural approach of functional and divisional resource allocation can take advantage of veterinary CE programs for the mutual benefit of CME programs.
Learning Through Lived Experience: Partnering with Patient Faculty in the Virtual Learning Environment
Authors: M. Suz Schrandt, JD, Founder & CEO, ExPPect, Steve Bender, President, FACTORx
Purpose/Problem statement
Much of the healthcare and research enterprise has embraced the concepts of patient engagement and patient-centered care, but these practices can be difficult to fully embed into CPD. The rapid transition to virtual learning brought about by the pandemic created a new opportunity for the meaningful involvement of individuals with lived experience into the creation and presentation of curriculum, in ways that in-person programming may be less able to accommodate. While many educational offerings endeavor to build provider capacity to engage in shared decision-making and co-production with their patients, fewer have involved patients as faculty members in the curriculum design, and even fewer have based curriculum on evidence from patient-generated data itself. The CME initiative described herein was a collaboration between clinician, patient, and research partners, providing practical guidance for clinicians to best support and foster high-quality care for their patients.
Approach(es)
For this CME initiative, focused on the use of biosimilars and biologics as treatment for rheumatoid arthritis (RA) and inflammatory bowel disease (IBD), an RA patient and an IBD patient, each with robust history and connection to their respective patient communities, partnered with the clinical faculty to design and present the program. The multistakeholder team drafted and executed a survey of 145 RA and 101 IBD patients, seeking to unearth patient experiences, knowledge, and feelings or beliefs about biosimilars. This analyzed data was used to contextualize the clinical educational content against the backdrop of patient information, communication, and treatment preferences. For example, free text responses that revealed common misconceptions about biologics and biosimilars provided critical insight for learners, to enable them to better explain and outline risks and benefits of treatment. This first-hand, lived experience of patients filled critical knowledge and practice gaps for learners seeking optimal shared decision-making approaches. The design of the educational module itself was also novel. Opening with concise clinical content about the RA and IBD disease processes and treatment options, the majority of the content was delivered through a moderated panel discussion between the patient and clinical faculty, reviewing and surfacing critical learnings from the survey data and offering ideas and solutions for navigating difficult patient/provider conversations and decision-making.
Evaluation/Outcomes Discussion
Through 7/12 of its lifecycle, the activity has generated more than 900 learners and 348 CME credit earners. Pre and post test scores have improved dramatically over the 6 clinical recommendations with pre scores ranging from 26-66% to post-scores of 91-100%. In one instance, the most popular pre-test answer was 66% for the incorrect therapy and post-scores increased to 100% for the correct therapy. A more complete assessment will occur upon activity expiration.
The goals of this project were two-fold: first to provide clinicians who treat RA and IBD patients with a better understanding of the manufacturing process for biologics and biosimilars and second, to present the major patient questions and concerns when it comes to switching from an originator therapy to a biosimilar so that both the clinicians and patients are better prepared for those discussions. The latter task would be nearly impossible without hearing directly from the affected patient communities, but doing so requires careful and intentional planning and effort. Involving patient faculty members as partners in the process from the beginning to the end ensures a consistent and constant patient presence as content is developed and delivered. Capturing data from a wide array of patients ensures representativeness of the information, and provides quantifiable evidence to underscore what could otherwise be disregarded as anecdotal patient insight. The pinnacle of the innovation in this approach however, was the intersection of the patient faculty with the survey process. Involving patient faculty in the design of the survey and review of the survey data ensured that the language was understandable, that patient-important questions were included, and that answer choices appropriately covered the full range of considerations. This rich patient engagement methodology was further enhanced through robust and iterative collaboration with clinician and researcher faculty members. This three-part approach could be widely adopted across an array of difficult-to-treat conditions to better equip clinicians with tools and capacity to engage in important and sometimes difficult conversations with their patients.
Key Learnings for CME/CPD Practice
As with any efforts involving patient faculty, there is always a learning curve for all involved. Thankfully, the co-creators of the initiative have long tenures in innovating CME programming and over a decade of experience incorporating and embedding the patient perspective and patient faculty members into curriculum development and presentation. With the pandemic and the need to dramatically shift all programming to virtual platforms, we realized this shift could be used to our advantage. Patients with chronic illness may have difficulty with travel, and the ability for them to participate through video conference alleviates many potential burdens. The other characteristic of virtual learning that can be difficult is the inability to interact with learners in the moment. Because of the structure of our program and the ability of the patient and clinical faculty to interact with one another in the panel discussion, it created the sense of engagement and interactivity even without the ability for learners to weigh in. The only unmitigable barrier to hosting this CME initiative in a purely virtual platform was the missed opportunity for learners to engage directly with patient faculty. In prior, similar educational activities created and presented by the co-creators of this CME initiative, learners have literally lined up to speak with the patient faculty at the conclusion of the live program and even remarked at the value and benefit of being able to speak with a "real" patient outside of the stressful confines of a healthcare setting.
The phenomenon of using real--not scripted or standardized--patients in medical education has gained critical acclaim and since the adoption of the ACCME’s Criterion 24, is increasingly recognized as a vital teaching tool. As early as 1978 with the World Health Organization's Alma-Ata Declaration, patients (and people in general) were decreed to have a right and duty to participate individually and collectively in the planning and implementation of their health care, which includes education and innovation in care and delivery. Despite an exploding landscape of best and promising practices in patient engagement in nearly every sector of medicine and research, an equally robust body of best and promising practices does not yet exist in continuing medical education and continuing professional development. Approaches such as ours, prioritizing and elevating patient-generated data and involving patient faculty as members of the team, are the path forward for making meaningful patient engagement in CME the norm rather than the exception.
Narrative Medicine for Spiritual Health and Enhanced Diversity, Equity and Inclusion Training Among Healthcare Professionals
Author: Elizabeth J. Berger, MS, APBCC, NBCC
Institution: Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Spiritual Health at Work
Purpose
The association of clinician well-being with patient perceptions and quality of care has been long established in the medical literature. Spiritual health, which may or may not include religious practice, is the component of mental health associated with a nourished sense of meaning, purpose and connectedness. It is a frequently overlooked component of well-being among physicians and an often unaddressed dimension of diversity, equity and inclusion programming. Transcending healthcare's cultural limitations with respect to spirituality is important to patient-centered care and to organizational and individual well-being.
Approach and Educational Design
Narrative medicine is a set of practices using media and reflective writing in a facilitated, secure environment. A 75-minute narrative medicine workshop can be structured as follows: Orientation and introduction (5); presentation of the artifact (15); discussion (20); writing to the prepared prompt (5); sharing of reflections (20); debrief/ Q and A (10). Narrative medicine workshops are effective whether conducted virtually or in person. Narrative medicine artifacts are selected to promote spiritual health in ways that are aligned with a consensus definition of spirituality from the Journal of Palliative Medicine: Spirituality: The aspect of humanity that refers to the way individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and to the significant or sacred (Puchalski et al. 2009).
Evaluation/Outcomes
Narrative medicine outcomes may be evaluated using a variety of qualitative and quantitative approaches as reflected in a 2020 BMJ systematic review of 55 programs (Remein et al.) https://bmjopen.bmj.com/content/10/1/e031568#T2
Narrative medicine has been associated with "a range of positive outcomes for health sciences professionals, including enhancing narrative competence, communication and empathy; detecting and mitigating burnout; fostering reflection with regard to professional identity formation; promoting team-building and facilitating teaching competencies." It can also promote spiritual health by bridging the disconnects between the existential crisis of illness and healthcare's Cartesian ideal of scientific mastery, between clinicians’ spiritual and professional lives, and ultimately, between the clinician and the patient.
Key Learnings for CME/CPD Practice
Opportunities for meaning-making are ever more important in the wake of COVID-19. Without pathologizing their experiences or calling competence into question, narrative medicine affords physicians a safe, academic framework for exploring their experiences, those of their patients, and belief systems beyond the medical model.
Participants are:
- better prepared to attend to their own well-being
- able to identify some of the barriers to spiritual health, the effect on patient care, and the connection to burnout (before/during COVID-19)
- afforded opportunities to deconstruct a persisting 20-century association of spirituality with anti-intellectualism and to reframe spirituality as an unrecognized dimension of diversity, equity and inclusion
- acquainted with the operational tenets of narrative medicine
In some instances, participants may be prepared with resources and rationale for instituting or expanding narrative medicine programs directed to spiritual health initiatives in their institutions.
Regularly Scheduled Series (RSS’s)—Reimagined
Author: Annette Mallory Donawa, PhD and Jennifer Turner
Institution: Thomas Jefferson University School of Medicine, Office of CPD
Background
Thomas Jefferson University’s Office of Continuing Professional Development (OCPD) examined the effectiveness of delivering regularly scheduled series (RSS) in virtual environments. According to the Joint Accreditation 2020 report, 4,199 RSS activities were delivered in 2020, a 50% increase in learner interactions in 2020 compared to 2019.
Theoretical Framework
OCPD conducted a comparative study focused on three phases: before, during COVID-19; and delivery plans for RSS education after COVID. Four major departments were targeted: 1) internal medicine; 2) oncology; 3) surgery and 4) orthopaedics.
Methods and Approach
This research project examined the effectiveness of the educational delivery method using online virtual platforms and learner perceptions of the quality of educational content for the virtual courses. Data elements were obtained from two surveys, one from planners and the other survey from participants. Data from participant survey will be shared at the conference.
Findings/Discussion
Preliminary data results (N=34) from planners convey the following:
- BEFORE COVID, 85% held in-person meetings; 0% used virtual formats; 15% used a hybrid format; and 0% used Enduring
- DURING COVID, 6% held in-person meetings; 85% used virtual formats; 9% used a hybrid format; and 0% used Enduring
- Education content was quality, 94% said Yes; 6% said No.
- Plans for delivering RSS AFTER COVID, 79% Yes; 21% said No
Transitioning from an In-person CME Ultrasound Point of Care Training to a Virtual CME-Tele-Ultrasound Point of Care Training during the COVID-19 Pandemic
Authors: Nilam J. Soni, MD, MS, Jeremy S. Boyd, MD, Gregory Mints, MD, Kevin Proud, MD, Trevor P. Jensen, MD, MS, Gig Liu, MD, Benji K. Mathews, MD, Christopher K. Schott, MD MS, Linda Kurian, MD, Charles M. LoPresti, MD, Phil Andrus, MD, Robert Nathanson, MD, Natalie Smith BS, Elizabeth K. Haro, MPH, Michael J. Mader, MS, Jacqueline Pugh, MD, Marcos I. Restrepo MD, MSc PhD, Brian P. Lucas, MD, MS
Purpose/Problem Statement/Scope of Inquiry
Competency in point of care ultrasound (POCUS) requires basic knowledge of ultrasound technology, skills in image acquisition and interpretation, and ability to integrate findings into clinical decision-making. Most practicing clinicians gain POCUS skills by attending in-person continuing medical education (CME) courses, and these courses have been shown to be effective.
Due to travel restrictions and physical distancing requirements during the COVID-19 pandemic, most in-person POCUS training courses were cancelled; however, the demand for POCUS training may have increased given the utility of POCUS in the care of COVID-19 patients. A major challenge in creating virtual POCUS CME courses is the need for hands-on training with live and simulation models with expert faculty guiding learners’ hand position and technique. Tele-ultrasound technology has been used to perform remote patient scanning, but few studies have described its use for virtual hands-on training of clinicians who are novice in POCUS use. No prior studies have described use of tele-ultrasound technology for hands-on POCUS training as part of an accredited CME course for practicing clinicians.
We converted an established in-person POCUS CME course to a tele-ultrasound course during the COVID-19 pandemic. The goal of the tele-ultrasound POCUS CME course was to provide the same educational experience, including hands-on training, using a virtual format. We compared the change in POCUS knowledge of learners, fulfillment of course objectives, and faculty and learner feedback of the in-person versus tele-ultrasound POCUS CME course.
Approach(es)/Research Method(s)/Educational Design
A retrospective observational study comparing an established in-person POCUS course in February 2020 (pre-pandemic) versus tele-ultrasound POCUS courses in July 2020 and February 2021 during the COVID-19 pandemic. The same POCUS educational curriculum was used for the in-person and tele-ultrasound courses, although the format of delivering educational content differed.
In-person Course
We held in-person POCUS courses every 6-12 months from 2013 until the COVID-19 pandemic in early 2020. These 2-day courses combined focused lectures, image review sessions, and hands-on scanning sessions. Both live models and simulators were used. A learner to faculty ratio of 3:1 or 2:1 was maintained for all hands-on training. Data from the most recent in-person course in February 2020 was used for comparison to the tele-ultrasound courses.
Tele-Ultrasound Course
To meet the ongoing demand of POCUS training during the COVID-19 pandemic, we converted our traditional 2-day in-person course into a 4-week tele-ultrasound course. While the number of CME hours from didactics and hands-on training stayed the same (16.25 hours), the curriculum was spread over 4 weeks for two reasons. First, learners and faculty needed additional time to become comfortable using the tele-ultrasound software. Second, our course coordinators were online to connect faculty and learners, initiate the hands-on scanning sessions, and troubleshoot any problems that arose during the session. Thus, we scheduled individual hands-on scanning sessions at different times, rather than all learners and faculty scanning simultaneously. The learner to faculty ratio was 2:1 or 1:1 for all hands-on scanning sessions. We utilized Reacts tele-ultrasound software (Philips & Innovative Imaging Technologies, Montreal, Canada). This software allowed simultaneous visualization of a learner’s hand position and ultrasound screen.
We piloted our tele-ultrasound course with 12 learners at 4 remote critical access hospitals in southeastern Alaska in July 2020, followed by a larger course with 43 learners from 14 different states in the United States and abroad in February 2021. Twenty-six experienced POCUS faculty specializing in internal medicine, hospital medicine, critical care, and emergency medicine from 15 different U.S. institutions provided virtual hands-on POCUS instruction by tele-ultrasound. Faculty and learners were scheduled for 2-hour hands-on scanning sessions that allowed for 60-90 minutes of actual scanning. Live models were relatives of learners, co-course participants, or volunteer staff or patients.
Learners completed pre- and post-course knowledge tests, CME course evaluations, tele-ultrasound course evaluations, and participated in a live post-course debriefing. The knowledge test included 30 questions focusing on fundamentals of ultrasonography, image interpretation, and integration of POCUS findings in clinical decision-making. Learners completed a standard CME course evaluation that gathered both quantitative and qualitative feedback after both the in-person and tele-ultrasound POCUS courses. Learners evaluated fulfillment of course objectives and quality of lectures and hands-on scanning sessions by rating their agreement with standardized statements on a scale of 1 to 5 (1 = “not at all” or “low agreement”; 5= “excellent” or “high agreement”). Qualitative feedback was gathered from learners of the in-person and tele-ultrasound courses regarding the teaching effectiveness of faculty for hands-on sessions, new knowledge or practice strategies gained, and practice changes implemented after attending the course. Qualitative data were collected from learners using free text boxes in the CME course evaluation and tele-ultrasound course evaluation, and during live post-course debriefing sessions. Faculty evaluated the tele-ultrasound course by completing the same tele-ultrasound course evaluation as learners that included faculty-specific questions and during a live post-course debriefing session for faculty.
Evaluation/Outcomes/Discussion
Pre and post-course knowledge test scores of learners from the in-person (n=88) and tele-ultrasound course (n=52) were compared. Though mean pre-course knowledge test scores were higher among learners of the tele-ultrasound versus in-person course (78% vs. 71%; p=0.001), there was no significant difference in the post-course test scores between learners of the two course formats (89% vs. 87%; p=0.069). Both learners and faculty rated the tele-ultrasound course highly (4.6-5.0 on a 5-point scale) for effectiveness of virtual lectures, tele-ultrasound hands-on scanning sessions, and course administration. Faculty generally expressed less satisfaction with their ability to engage with learners, troubleshoot image acquisition, and provide feedback during the tele-ultrasound course.
For many learners, the primary reason to attend an in-person POCUS CME course was the opportunity to practice hands-on scanning on live models and ultrasound-guided procedures on simulators under the guidance of expert faculty. We have demonstrated that hands-on scanning is feasible using tele-ultrasound technology, and a tele-ultrasound POCUS CME course can improve learners’ post-course knowledge to a similar level as an in-person course. By improving learners’ access to expert faculty for mentored scanning, tele-ultrasound can help bridge the gap in POCUS training for physician in-practice in the coming years.
Key Learnings for CME/CPD Practice
Compared to a traditional in-person POCUS CME course, a tele-ultrasound course appeared to be as effective for improving POCUS knowledge post-course and fulfilling learning objectives for novice POCUS users. Our findings can serve as a roadmap for educators seeking guidance on how to develop a tele-ultrasound POCUS training course whose demand will likely continue after the COVID-19 pandemic.
Full text article available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8419826/
Reimaging Bias: Making Strange with Disclosure
Authors: Morag Paton MEd, PhD(C), Eleftherios K. Soleas, MEd, PhD, Brian D. Hodges, MD, PhD
Institution: University of Toronto, Temerty Faculty of Medicine; Queen’s University, Faculty of Health Sciences
Purpose
To present at this conference, we were required to disclose potential conflicts of interest. It is a standard and somewhat routine protocol in most Canadian CPD organizations and perhaps elsewhere. This process is intended to identify COI and minimize bias to increase objectivity in academic presentations. By disclosing conflicts of interest, it seemingly authenticates the learning that follows. The audience is assumed to accept that by disclosing potential financial COIs, the presentation is cleansed of bias or that the forms of bias contained within are not of material significance.
Academic presentations in CPD often begin with a declaration of real or potential conflicts of interest (COI) utilizing a three-slide template or a similar standardized display. The template and similar protocols exist to assure learners that the content that follows has been screened, is notionally bias-free, and without financial or other influence that might negatively impact health provider behaviour.
Approach
We suggest that there is a potential problem: the focus on financial COI is too narrow and may do little to confront the issue that bias is a much larger concept and that many forms of bias (beyond financial COIs) can have devastating effects on patient care. We argue that other forms of bias, arising from the perspectives of the presenter, can also potentially change provider behaviour. Implicit biases, for example, affect relationships with patients and can lead to negative health outcomes.
While CPD program participants perceive low levels of bias and commercial influence, there is increasing concern about bias in health care. Potential biases among healthcare providers have been identified, for example:
- Individuals with limited English proficiency are readmitted to hospital after discharge at higher rates compared with those without this limited proficiency, compromising patient care.
- Women are being underdiagnosed or mis-diagnosed in cardiology.
- In the United States, racialized communities receive lower-quality care compared with white Americans.
- Indigenous Peoples in Canada continue to experience structural and experiential inequities related to healthcare.
These bias may be implicit. Implicit biases are the unconscious activations of stereotypes that have developed through one’s own life experiences, and “can be automatically activated in ways that bypass deliberate thought and influence one’s judgment in unintended and unacknowledged ways.”16, p.1505
Outcomes and Discussion
Continuing professional development providers can begin to identify opportunities to bring bias literacy into the education presentation and CPD programming contexts, augmenting our traditional focus on financial bias.
We hope to open dialogue around this issue by ‘making the familiar strange’, by asking education organizers and providers to question these standard disclosures. We call CPD to action to reimagine the process of disclosure of COIs. We seek to expand reflection on, and disclosure of, perspectives and biases that could impact CPD learners as one dimension of harnessing the power of education to decrease structural inequities.
Key Learnings for CME/CPD Practice
1. Don’t stop at a financial COI declaration form, encourage dialogue and more open conversations about biases
2. Speakers could more explicitly disclose perspectives or standpoints that may change the attitudes or behaviors of their audiences.17-19
3. Providers could ask that in addition to positive findings, limitations of studies cited in programs be included in educational content.
4. Encourage and train for ongoing reflection through explicit training in implicit bias (although this has its limits too)20
5. Equip health providers and peer reviewers with critical appraisal tools
6. Encourage peer reviewers to consider potential implicit biases when reviewing
For more detail and elaboration: please see our published paper at the Journal of Continuing Education in the Health Professions: https://journals.lww.com/jcehp/Abstract/2021/04120/Reimagining_Bias__Making_Strange_With_Disclosure.10.aspx
Pivoting CPD During the COVID-19 Pandemic: A Scoping Review of Emerging and Amplified Trends and Innovations
Authors: Sophie Soklaridis, PhD, Mushfika Chowdhury, Paul Mazmanian, MD, Martin Tremblay, PhD, Mary G. Turco, EdD, Betsy Williams, PhD, Reena Besa, MLIS, Sanjeev Sockalingam, MD
Institutions: Centre for Addiction and Mental Health, Toronto, Ontario, Canada; Department of Medicine, Dartmouth-Hitchcock Medical Centre/Geisel School of Medicine at Dartmouth, Lebanon, NH, USA; Fédération des médecins spécialistes du Québec, Montréal, Québec, Canada; Department of Preventive Medicine and Community Health, Virginia Commonwealth University, Richmond, Virginia, USA; Professional Renewal Centre, Lawrence, KS, USA.
Purpose/Problem Statement/Scope of Inquiry
With limitations on travel and physical distancing, a burgeoning of new information about the management of COVID-19 and an increase in clinical workload, there has been a swift effort to accelerate the development of virtual teaching and learning environments to continue offering CPD throughout the pandemic1. The urgency for rapid and novel adaptations to CPD resulted in both an opportunity for innovations and a deep contemplation on which trends will continue after the most acute phases of the pandemic. In this narrative scoping review, we explored the adaptations and innovations in CPD, strengthened or newly created, due to the COVID-19 pandemic. The purpose of our narrative review was to use a systematic approach to synthesize the findings of studies from March 2020 to July 2021 to examine how this unprecedented time led to adaptations and novel ways of thinking that now define the landscape of CPD.
Approach(es)/Research Method(s)/Educational Design
We used the Arksey and O’Malley’s scoping review framework2 and the PRISMA extension for scoping reviews to ensure the reporting and synthesizing of the evidence met the current standards for reporting on knowledge synthesis research. Our review added to both Gordon et al.’s (2020)3 systematic review of the developments in medical education in response to the COVID-19 pandemic (to May 2020) and the updated publication of this review by Daniel et al (2021)4 (to September 2020). We included all article types such as opinion, commentaries, and editorials- which were excluded in the previous two reviews- because these types of articles provided perspectives from experts in the field regarding current issues and where the field of CPD may evolve in the near future. Our research addressed the following question: What do studies in CPD show us about trends and innovations as a result of COVID-19? Our scoping review answered the following questions: 1) what types of and adaptations to CPD innovations are described? 2) what are the future innovations in CPD?
Evaluation/Outcomes/Discussion
We identified 190 articles to include in our final analysis. Of the total 190 articles included, less than one fourth offered a theoretical or evaluation framework. We identified 123 articles that described three types of adaptation to CPD innovations: 1) The creation of new on-line resources, 2) The increased use of existing online platforms/software to deliver CPD, and 3) The use of simulation for teaching and learning. We identified 65 articles that described or explained five future innovations that will shape CPD initiatives beyond the pandemic: 1) empirical research on effectiveness of virtual learning; 2) novel roles and ways of thinking; 3) learning from other health disciplines and moving beyond medicine; 4) formation of a global perspective; and 5) emerging wellness initiatives for health professionals
Key Learnings for CME/CPD Practice
- New modalities to deliver CPD, such as social media are on the rise. However, in our review, no articles offered theoretical frameworks or a discussion of pedagogical considerations to using this medium for teaching and learning
- CPD may need to provide training in emerging roles related to on artificial intelligence, data science and digital technology, which in many institutions has remained outside of health professions education
- Based on the literature, we can anticipate the need for CPD research to show how initiatives can support health professional wellness due to issues resulting from the pandemic
- The future of CPD research and scholarship will require a focus on implementation research to better understand and inform the improvement of virtual learning and hybrid models
Key References
1. Thakur A, Soklaridis S, Crawford A, Mulsant B, Sockalingam S. Using Rapid Design Thinking to Overcome COVID-19 Challenges in Medical Education. Academic medicine : journal of the Association of American Medical Colleges. 2020;01(PG-). doi:http://dx.doi.org/10.1097/ACM.0000000000003718.
2. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19-32. doi:10.1080/1364557032000119616.
3. Gordon M, Patricio M, Horne L, et al. Developments in medical education in response to the COVID-19 pandemic: A rapid BEME systematic review: BEME Guide No. 63. Medical teacher. 2020;42(11):1202-1215. doi:10.1080/0142159X.2020.1807484.
4. Daniel M, Gordon M, Patricio M, et al. An update on developments in medical education in response to the COVID-19 pandemic: A BEME scoping review: BEME Guide No. 64. Medical teacher. 2021;43(3):253-271. doi:10.1080/0142159X.2020.1864310.
Success of Virtual Platform for an Established “Train the Trainer” Course
Authors: Amber Shada, MD, Jaime Sanchez, MD, Yong Choi, MD, Erin Schwarz, BA, John T. Paige, MD, Jonathan Dort, MD, Lisa Moudgill, MD, Greta Bernier, MD
Background/Problem
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) uses the Laparoscopic Colectomy Train the Trainer (Lapco TT) framework for standardization of instructor training in preparation for hands-on surgical skills courses. Lapco TT is a faculty development program designed to improve and standardize the quality of teaching technical skills to surgical learners. The curriculum focuses on teaching structure, skills deconstruction, trainer intervention framework, and performance enhancing feedback. A halt in the in-person Lapco TT courses due to the Coronavirus Disease 2019 (COVID 19) pandemic necessitated creation of a virtual alternative. We investigated the effectiveness of this virtual Lapco TT course.
Methods
Adaptation of the in person Lapco TT course to the virtual format retained the majority of content as well as the 4:6 instructor to participant ratio. The virtual platform and simulators chosen allowed maximal interactivity and ease of use. After participating in the day and one half course, participants completed an 8-item post-course survey using a 5-point Likert scale related to the training experience. In addition, they had the opportunity to provide answers to several open ended questions regarding the course. For the survey, frequency counts provided an assessment of each item. For the open questions, qualitative analysis included determination of themes for each question. Frequency counts of each theme provided quantitative analysis.
Outcomes
Thirty-six participants completed a Lapco TT virtual course (six sessions of six participants). Of this number, 32 participants completed post-course surveys and questions. All the participants completing the survey would very likely or definitely (Likert scale 4, 5) recommend the course to a colleague and incorporate the teaching in their practice. The majority of participants completing open-ended questions felt the virtual course format was effective; half thought that post-course follow-up would be useful. Technical concerns were an issue using the virtual format.
Key Learnings for CME/CPD Practice
A virtual Lapco TT course is feasible and well received by participants. It presents a potentially more cost-effective option to more traditional educational formats for faculty development.
Disclosures
The September 2020, November 2020, February 2021 and May 2021 virtual TT courses were supported by a grant from the SAGES Foundation and medical education grants from Applied
Medical and Ethicon USA / Johnson & Johnson Medical Devices Co. The July 2021 and September 2021 virtual courses were supported by a grant from the SAGES Foundation and by SAGES.
Perspectives and Innovation in Educational Design from the GAME Futurist Forums
Authors: Dale Kummerle PharmD, Celeste Kolanko MEd, Suzanne Murray
Institution: Global Alliance for Medical Education (GAME)
Purpose/Problem Statement/Scope of Inquiry
GAME leaders believe there remains a lot of interest in the future of lifelong learning (LLL) in healthcare and work to understand the trends continuously ongoing by many professionals and organizations globally. The first two Futurist Forums sought to identify and understand the most important trends and even identified potential solutions. The purpose of the next Futurist Forum is to explore and implement the previously identified solutions in regional “Innovathon” teams (see the educational design section). As the world returns to the possibility of live meetings, a hybrid instructional design will be utilized for maximum impact, flexibility, and engagement, with regional teams coming together at the hybrid meeting, then working independently over many months, and finally reconvening virtually to share their work and findings.
Approach(es)/Research Method(s)/Educational Design
Findings from the first Futurist Forum have been published in JECME* and are, along with the draft manuscript of the 2nd Futurist Forum, the foundation of the themes and solutions that will be implanted in the Innovathon. A high-level summary of these publications was presented to the audience as a part of the presentation. The key themes of the 2nd Futurist Forum (Futurist Mindset, Technology and Human Touch, and non-traditional collaborations) provided many interesting perspectives from around the globe and how they may or may not impact lifelong learning in healthcare.
While the approach taken for the 2022 Futurist Forum is still in full development, it will focus around a learner’s journey, with the start of journey reengaging the learners with the skill of the futurist mindset. Attendees at the live hybrid meeting will be introduced to the other major themes, and start to build the trust necessary for the intensive Innovathon learner’s journey. The learners will be encouraged to sign up as teams for a multi-month “Innovathon” based in their region of the world, and focus on initial project brainstorming and team building. Loosely based on the idea of a hackathon, regional teams, facilitated by a member of the Futurist and Innovations Committee, will engage each other regularly on a selected themes/solutions that resulted from discussion of the previous Forums. Results from the solution implementation of these Innovathon teams will be presented at a follow up virtual meeting in 2023.
Evaluation/Outcomes/Discussion
The current environment for lifelong learning in healthcare has changed dramatically over the last year, impacted by the global COVID-19 pandemic. Many trends identified during the first Futurist Forum (and published) were accelerated significantly, as institutions and organizations moved to address the needs of learners during a period where social distancing and quarantine necessitated by COVID-19 cancelled most live meetings. Virtual meetings via technological platforms became the norm immediately, versus the prior 5 to 10 years trending information. Analysis of the virtual meetings showed a significant increase in attendance, particularly by learners in other regions and whom may not have attended due to cost, travel, and/or time requirements. We believe, though, that the world is forever changed and we cannot move back to only live meetings if we want to advance lifelong learning in healthcare world-wide. We look to understand innovation in this new reality from the learner’s perspective through brainstorming. What does innovation mean to them, how do they innovate, and what is the most innovative educational activity in which they have participated? Lastly, we want to show, through the Innovathon learner’s journey, how these solutions can accelerate trends for the betterment of lifelong learning in healthcare.
Key Learnings for CME/CPD Practice
Exploring and addressing future trends in lifelong learning in healthcare will help learners develop a futurist mindset and ease the fear of change that is likely to occur over the next 10 years. Demonstration projects like the Innovathons will help accelerate solutions to identified barriers to change and improve overall outcomes in learning and healthcare. Professionals in Healthcare are notorious for a wait and see attitude, but we believe it is the responsibility of the professionals educating healthcare learners to assist in acknowledgment of future trends and subsequent embracing of the change with concrete solutions.
*Suzanne Murray, Jur Koksma, Aviad Haramati, Eric Bonnefoy, Nabil Zary, Werner Bill, Olaf Wolkenhauer, Susanna Price & Dale Kummerle (2021) Imagining the Future of Learning in Healthcare: The GAME 2019 #FuturistForum, Journal of European CME, 10:1, DOI: 10.1080/21614083.2021.1984076
Professional Title Use and Gender Representation During Grand Rounds and Invited Lectureships Across Specialties
Authors: Alexandra Hernandez, MD, MCR, Mollie C. Marr, PhD, Alexandra Pincus, PhD, Karen Brasel, MD, MPH
Institutions: Oregon Health & Science University, University of Washington
Background/purpose/inquiry question
Despite the growing number of women entering medicine, gender disparities persist. Studies show that women are underrepresented as speakers from institutional grand rounds to plenary speakers at national medical conferences and are less likely to be introduced by their professional title. The objective of the study is to examine gender-related disparities in representation and title use during grand rounds and invited lectureships.
Theoretical framework(s)
To address gender disparities in representation and title use, our study incorporates specialty and training level to better understand the professional context.
Methods
This is a retrospective, observational study of video archived grand rounds across six specialties at a large academic medical center. Summary and chi-squared statistics and logistics regression were used to describe representation and title use as it related to gender, specialty, and training level.
Results/findings
Women were underrepresented as speakers during Grand Rounds, and a greater proportion of female speakers were trainees when compared to male speakers. There were significant specialty-related differences in title use during introduction.
Discussion
Departmental policy and intervention appears to impact title use during introduction and has the potential to reduce gender disparities. Medical hierarchy evidenced by training level has asignificant impact on the use of titles during introduction.
Limitation
The study is a single institution study.
Impact/relevance to the advancement of the field of CME/CPD
Our study demonstrates potential solutions to a known academic challenges for women. Further evaluation with inter-institutional collaboration will improve our ability to understand cultural factors and their impact on equity in academic medicine.
From SWOT to Strategic Planning: A team-based approach
Author: Annette Donowa, PhD
Institution: Thomas Jefferson University School of Medicine, Office of CPD
Background
The Office of Continuing Professional Development (OCPD) at Thomas Jefferson University engages in strategic planning by completing a team-based strengths, weaknesses, opportunities, and threats (SWOT) analysis. The SWOT process supports professional development for the CME/CPD team, which is aligned with accreditation criteria: C34 and JAC15.
Theoretical Framework
A manual thematic analysis was conducted to code qualitative data, focusing on key words and themes from the staff’s responses. Using inductive coding, themes emerged for each category.
Methods and Approach
Staff were introduced to the SWOT analysis method during monthly staff meetings. It was explained that strengths and weaknesses were focused on internal processes and opportunities and threats focused on external matters. Staff had three to four months to submit their individual SWOT analysis and were encouraged to be honest and transparent.
Inductive coding was used to determine the themes that emerged for each category by the Assistant Provost. Teams were developed for themes in each category. Teams met for seven months. Team projects will be shared at the Staff Retreat on 12/17/21. Results and feedback will be included in the strategic plan.
Feedback from annual key stakeholder surveys will be included in the strategic plan. In addition, OCPD’s strategic plan is aligned with the four academic pillars championed by Jefferson’s Provost of Academic Affairs strategic plan. Ensuring alliance with the institution’s strategic plan
Findings/ discussion
The following themes emerged from the qualitative analysis:
- Strengths: staff, quality education/service, faculty, Joint Accreditation (JA)
- Weaknesses: LMS, lack of resources, lack of internal communication, standardized fee structure
- Opportunities: JA, expand institutional brand, attract global/diverse audience
- Threats: On-campus space, faculty education on accreditation, local competition
Impact/relevance to the advancement of the field of CME/CPD
Conducting a team-based
SWOT analysis can inform CME/CPD’s departments’ strategic plans. It is
imperative to use a team-based approach when strategic planning to ensure
buy-in from staff and to support professional development for the CME/CPD team.
Action items can be aligned with goals and objectives to guide the performance
review process.
Current Issue - Spring 2022
-
08 Apr 2022 11:32 AM
-
08 Apr 2022 11:31 AM
-
08 Apr 2022 11:29 AM
-
08 Apr 2022 11:27 AM
-
08 Apr 2022 11:24 AM
-
08 Apr 2022 11:22 AM